Looking for Expert-Level VA Claim Answers?📱Call Us Now! 737-295-2226
“Is PTSD a disability?” Many veterans ask this question, and the answer is absolutely yes. Post-traumatic stress disorder is not only disabling to many veterans, but is an official ratable disability that can be service-connected for compensation from the VA.
The Department of Veterans Affairs recognizes PTSD as a mental condition that can result from military service, and will therefore compensate veterans for PTSD if it’s service-connected and a claim is filed.
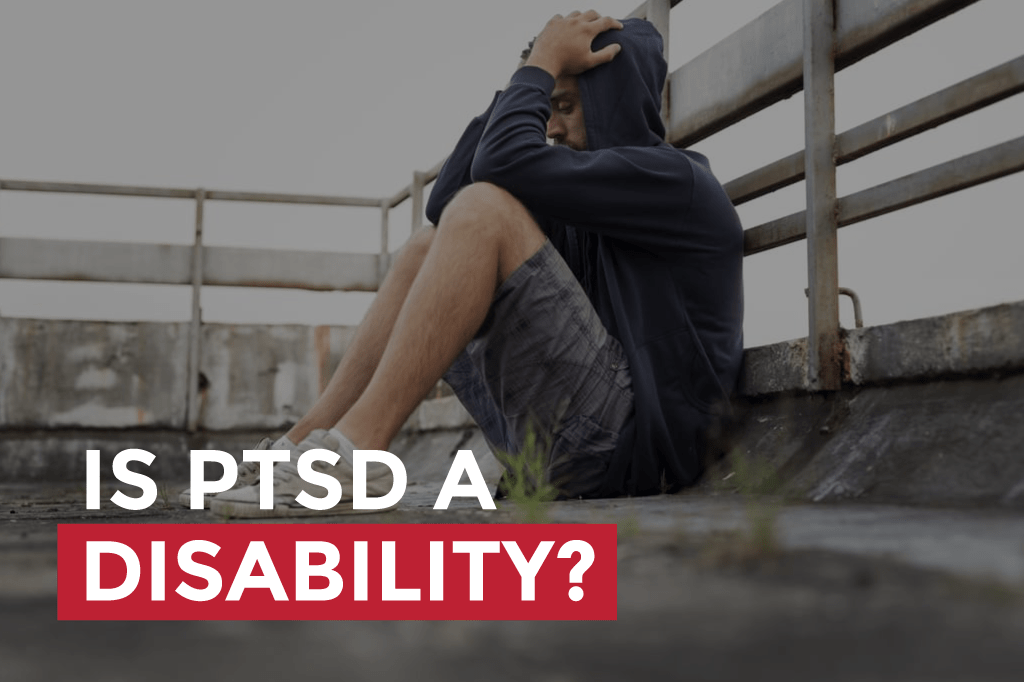
“Is PTSD a disability” is only the tip of the iceberg when it comes to questions about this often distressing condition. The prevalence of PTSD in veterans is high, and since it is a disability it’s important to know not only how to get support and treatment but compensation for it. Below, we cover common questions about PTSD, particularly in veterans, as well as VA rating and compensation for PTSD.
You DESERVE a HIGHER VA rating.
Take advantage of a VA Claim Discovery Call with an experienced Team Member. Learn what you’ve been missing so you can FINALLY get the disability rating and compensation you’ve earned for your service.
- What is PTSD?
- Post Traumatic Stress Disorder (PTSD) VA Disability Claims Rating Scale Explained!
- PTSD Symptoms
- PTSD Treatment
- PTSD in Veterans
- Is PTSD permanent?
- How does the VA Rate PTSD?
- What is the average disability rating for PTSD?
- Is 70% PTSD a permanent VA disability? What about 100%?
- What is the process for filing a PTSD VA disability claim?
- How do you prove VA disability for PTSD?
- What does PTSD VA disability pay?
- Can I work with a PTSD VA rating?
- How can I help a veteran with PTSD?
- How can I obtain a Service Dog for PTSD?
- Can I buy a gun with a PTSD VA rating?
- We’ve helped many thousands of veterans obtain or increase a VA disability rating for PTSD.
- MAKE SURE YOU GET ALL THE BENEFITS YOU DESERVE
- ABOUT THE AUTHOR
What is PTSD?
Posttraumatic stress disorder (PTSD) is a mental health condition that can develop in response to a stressor or trauma—a shocking, terrifying, or dangerous event or experience. It can be triggered either by experiencing it or witnessing the event.
When we experience or witness a traumatic event or stressor, our bodies respond with a cascade of reactions that put us in “fight or flight” mode. Stress and trauma trigger the release of stress hormones in the body, such as norepinephrine and adrenaline. This cocktail of hormones provides a quick burst of energy. The heart rate increases, and memory may be negatively affected.
The “fight or flight” response has an evolutionary purpose, and is part of our normal survival instincts. It allows us to identify a threat and be ready to fight it or run away from it. When triggered occasionally, under normal circumstances, the body and brain can generally recover and restore from the stress. We metabolize the cocktail of hormones within 12-30 hours.
But repeated frightening or distressing events and experiences can eventually rewire the brain to remain on alert even when there’s no danger. PTSD creates chemical changes and imbalances, and enlarges the amygdala, the part of the brain that controls emotional responses. When stress signals and warnings are sent throughout the body on an ongoing basis, it wreaks havoc on both body and mind.
Depending on many factors, everyone has a threshold for how much of this “fight or flight cocktail” the body can experience without triggering deeper, wider-ranging and more lasting effects.
Once we pass our unique particular threshold or tolerance for this cascade of chemicals, the body will begin to rewrite the nervous system to prepare for the more frequent threats the body has come to perceive as likely. Activating this “threat perception system” means the individual is now hypersensitized to stressors, whether or not a threat is actually imminent.
In addition to whatever unique psychological and physical characteristics and experiences might play into an individual’s development of PTSD, the sheer number of repeated “fight or flight” episodes to which a veteran is exposed sets the stage for the condition. The average person may experience two to four of these traumatic events over a lifetime, while—like first responders—veterans are likely to experience hundreds.
PTSD has been known by many names in the past, such as “shell shock” during World War I and “combat fatigue” after World War II. Although PTSD certainly does not happen only to veterans, the fact that it was identified by these names indicates just how prevalent it has long been in the veteran community.
Post Traumatic Stress Disorder (PTSD) VA Disability Claims Rating Scale Explained!
PTSD Symptoms
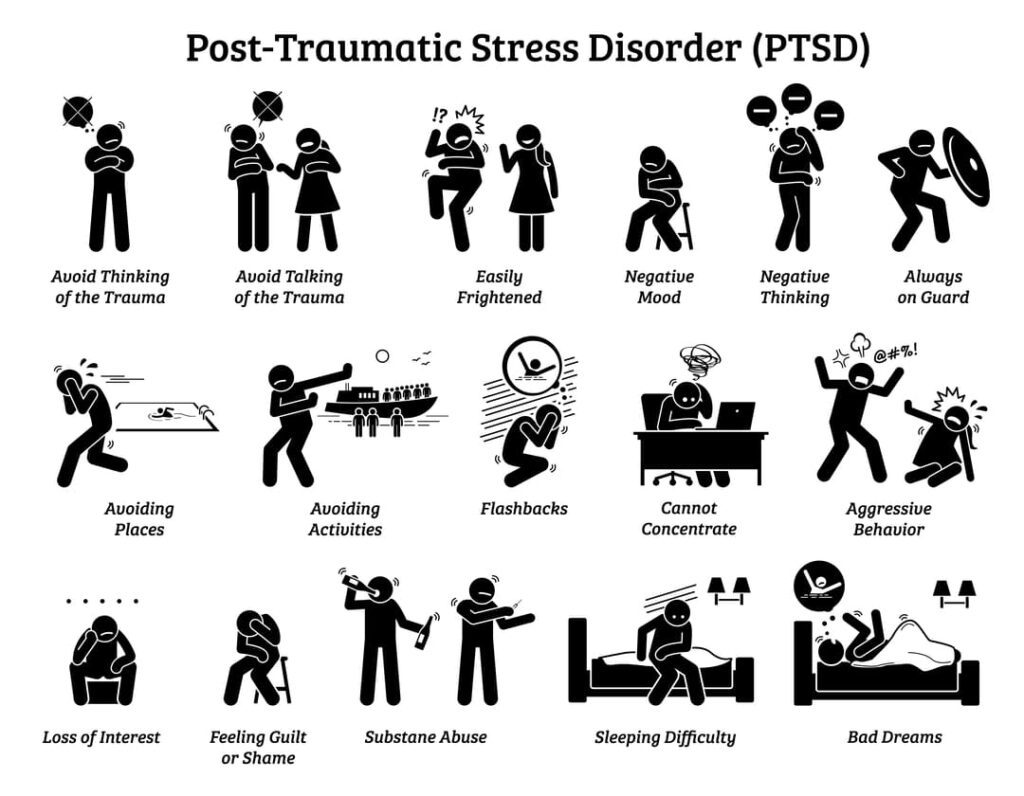
According to the Mayo Clinic, “Symptoms of PTSD may include flashbacks, nightmares and severe anxiety, as well as uncontrollable thoughts about the event.” People with PTSD may have intense, disturbing thoughts and feelings. They may experience feelings of isolation, irritability, sadness, fear, anger, and guilt, as well as insomnia and difficulty concentrating.
These symptoms usually have a significant impact on day-to-day life.
People with PTSD may avoid situations or people that remind them of the traumatic event, and they may have strong negative reactions to something as ordinary as a loud noise or an accidental touch. They may feel detached or estranged from other people, which makes relationships challenging.
PTSD symptoms are generally categorized into four types:
- Avoidance: Sufferers of PTSD often find it overwhelming to confront anything that reminds them of their traumatic experiences. Veterans who have PTSD may even isolate themselves to avoid any reminders of their trauma, including people, events, places, and certain objects.
- Cognitive and mood symptoms, or negative thoughts and feelings: People with PTSD may feel guilt and shame surrounding their trauma They may have memory issues, including trouble recalling the event. Self-image can be negatively affected. They may feel worried or depressed. Cognitive symptoms can in some cases extend to out-of-body experiences, depersonalization or derealization).
- Arousal: People with PTSD may feel a sense of constant anxiety or being hypervigilant. They may feel “on edge” all the time, even if nothing is wrong. They might be intensely startled by any stimuli that resembles or has association with the trauma, and easily angered. They may be hypersensitive to sounds, lights and touch.
- Reliving: One of the most common types of PTSD symptoms is the intense memories that come back long after a traumatic experience has occurred. These memories may come in the form of flashbacks or nightmares, and they often make it difficult for Veterans with PTSD to function during the day and sleep well at night. Many Veterans with PTSD have insomnia as a result.
The amount of time it takes for PTSD symptoms to manifest varies widely. Signs of PTSD might appear three months after experiencing a traumatic event or three years. Additionally, the intensity of symptoms may fluctuate.
PTSD symptoms occur on a spectrum. Some veterans with PTSD might require hospitalization, medications or extensive treatment to address symptoms; others may function adequately with therapy or counseling. Research shows that PTSD is significantly associated with suicide attempts.
PTSD Treatment
“Fighting” PTSD is not a question of strength or will. Once the brain has rewired the nervous system and created an enlarged amygdala, chemical imbalances and other brain changes, time alone will not heal or “fade” the condition. In fact, untreated PTSD over time often gets worse. Obtaining treatment and support is paramount.
PTSD can be successfully treated, however, even if it develops years after a traumatic event.
A diagnosis of PTSD requires a discussion or consultation with a trained and licensed mental health professional. Once diagnosed, veterans can get the PTSD treatment they need.
Treatment may depend in part on the type and severity of symptoms, how soon they occur after the traumatic event, and how long symptoms have progressed without treatment. Different individuals often respond differently to treatments as well, although some kind of therapy or counseling is recommended for most PTSD patients.
While medication helps many, it doesn’t work for everyone. Some veterans benefit from alternative treatments such as EMDR (Eye Movement Desensitization and Reprocessing, a psychotherapy treatment designed to alleviate the distress associated with traumatic memories). Some find relief by practicing yoga or meditation, participation in art or music, being outdoors in nature, in the company of animals, or in support groups.
The VA offers various forms of therapy to veterans, including family therapy. The VA also offers both a directory and a map that shows where PTSD resources are available by state.
The National Center for PTSD has a database of healthcare providers who are available to help.
PTSD in Veterans
Posttraumatic stress disorder (PTSD) and depression are two of the most common mental health conditions to which veterans are vulnerable after their service.
According to the U.S. Department of Veterans Affairs, 11-20 out of every 100 veterans experience post-traumatic stress disorder, and many experts believe that number is actually much higher. Because so many veterans either don’t realize the extent of their injuries, or don’t seek diagnosis and treatment due to stigma and fear of repercussion, PTSD often goes undiagnosed.

PTSD is the sixth most-rated disability among veterans. 2018-2019 VA data shows that mental health conditions including PTSD were among the top three most compensated VA claims for all veterans across all demographics. The VA compensates more than 800,000 veterans for symptoms of PTSD at some level.
PTSD in veterans can have both combat and non-combat in-service stressors. These can include exposure to death, threatened death, actual serious injury, threatened serious injury, actual sexual violence and threatened sexual violence.
In-combat stressor examples include rocket fire, IED explosions, enemy ambushes, any other kind of armed attack, plane crashes, or witnessing the death of a service member during deployment under any circumstances.
Non-combat PTSD stressors include events such as military sexual trauma (which can include but is not limited to either experiencing or witnessing sexual misconduct), service-member suicide, serious car accidents, or training accidents, among others.
Many veterans assume that if they have not experienced trauma in combat that it “doesn’t count.” This is absolutely untrue.
Is PTSD permanent?
There is no outright cure for PTSD, but many veterans can live functional and even satisfying lives with treatment and support that’s appropriate to the individual’s case. While the condition may be “permanent” in the sense that it’s rarely 100% gone, with the right help it can cease to play a dominant role in daily life.
Every PTSD patient’s needs are unique, but treatment almost always consists of psychotherapy, such as cognitive therapy, exposure therapy and regularly meeting with a psychiatrist, psychologist, therapist, or counselor. In some cases, medications may be used along with psychotherapy to help alleviate the effects of PTSD. Complementary medicine provides relief for many.
Many people wonder “Is PTSD a long-term disability?” In some cases, particularly when it’s not treated, PTSD can last a very long time, even for a veteran’s entire life. Many people find that symptoms may increase when they encounter reminders of their traumatic events. Anniversaries of the event, for example, are commonly difficult times.
Most people with longstanding PTSD find that the symptoms are not consistent or linear in severity. For some people, PTSD symptoms do gradually fade over time. Much depends on the individual’s physical and mental health, background and experience prior to the trauma(s), the nature of the trauma (not only what it was, but how long it lasted or how many instances), and the level of impairment. These variables should be considered in choosing approaches to treatment and support.
How does the VA Rate PTSD?
The VA lists PTSD as a “mental disorder due to traumatic stress.”
The VA will assign a disability rating based upon the severity of your PTSD, with criteria related to your level of occupational and social impairment. If you are considered service-connected, your PTSD may be rated by the VA at 0%, 10%, 30%, 50%, 70%, or 100%.
What is the average disability rating for PTSD?
The average PTSD rating is 70%. Overall, 53.81% of veterans with a PTSD rating are either rated at 50% or 70%. Also, more than 1,754,644 veterans had a PTSD rating between 0% and 100%.
21.9% of all disabled veterans receiving disability compensation from the VA have a service-connected rating for PTSD of 0% or higher. 59.3% of all veterans with a VA mental health rating are rated for Post Traumatic Stress Disorder.
Is 70% PTSD a permanent VA disability? What about 100%?
It can be. Although the terms “Permanent” and “Total” are often discussed together, it is possible to have a permanent disability that is not totally disabling. For example, a veteran may have a permanent disability (such as PTSD) at 70%, but the PTSD is not “total” because it is less than 100%.
A 100 percent rating for PTSD is a total rating. However, for PTSD to be permanent, it must be stated by the examiner that the PTSD is static and has no likelihood of improving over the veterans life..
(A permanent and total disability rating is always applied to the veteran’s overall disability picture, to include his or her other service-connected disabilities. Typically, all of the veteran’s service-connected disabilities will also have to be labeled as static by an examiner with no likelihood of improving over the veteran’s life.)
The 70% PTSD rating is marked by very severe symptoms and represents a big jump from the 50% level.
See our post “Permanent and Total Disability from the VA” for more general information. Or visit VA.gov.
What is the process for filing a PTSD VA disability claim?
Once you’ve answered “is PTSD a disability?” and you know that the VA does consider it a disability, the next question is often “how do I get a VA rating for PTSD?”
The process of filing a disability claim for PTSD includes all of the essential steps required when applying for any disability benefits from the VA. To file a claim with the VA,. you’ll always need to show three things: a nexus (link to service) for service connection, a current diagnosis (within 12 months) and medical evidence. The evidence must show the link between an in-service event and the disability (that it either caused or aggravated the disability).

Before filing, review the PTSD disability rating system to familiarize yourself with how the level of disability for PTSD is determined.
It’s especially critical that you support your claim with the applicable documentation to obtain the highest level of disability your case deserves, and therefore the highest monthly benefit amount. The VA will use medical evidence to determine the severity of your PTSD and assign your rating.
Use Statement in Support of Claim (VA Form 21-4138). Also, consider “buddy statements” and other layperson testimony from friends and family (use VA Form 21-10210 Lay Witness Statement) to support your case, explaining the full extent of your PTSD and how your brain injury affects your daily life.
You’ll also need to file VA Form 21-0781 (PTSD Stressor Form), which is used to verify the stressor. This is a requirement for PTSD claims. Alternatively, you may file VA Form 21-0781a, which is used to verify the stressor event for PTSD secondary to a personal trauma or sexual assault.
If the claimed stressor is verified with a current diagnosis and evidence of nexus, VA will schedule you for a Compensation and Pension (C&P) exam, and the C&P Examiner will complete the Disability Benefits Questionnaire (DBQ) for PTSD Initial.
How do you prove VA disability for PTSD?
PTSD is unique among veteran disability types because of the importance placed on stressors in diagnosing PTSD. As with all VA claims, you need to establish a service connection between your disability and your time in service. With a PTSD claim, you need to establish a stressor or stressors that qualify you for a diagnosis of PTSD.
As mentioned, these can be combat or non-combat stressors and can include sexual trauma.
As most military personnel and veterans know, many occurrences during military service are never documented or recorded. As a result, it can be very difficult to prove that a stressor took place. A 2010 VA rule makes it somewhat easier to prove that a stressor event happened during service.
Under the new regulation, if a veteran’s claimed stressors are related to the fear of hostile or military or terrorist activity, then he could qualify for PTSD based on the following stated by the Code of Federal Regulations (CFR):
If a stressor claimed by a veteran is related to the veteran’s fear of hostile military or terrorist activity and a VA psychiatrist or psychologist, or a psychiatrist or psychologist with whom VA has contracted, confirms that the claimed stressor is adequate to support a diagnosis of posttraumatic stress disorder and that the veteran’s symptoms are related to the claimed stressor, in the absence of clear and convincing evidence to the contrary, and provided the claimed stressor is consistent with the places, types, and circumstances of the veteran’s service, the veteran’s lay testimony alone may establish the occurrence of the claimed in-service stressor.
For purposes of this paragraph, “fear of hostile military or terrorist activity” means that a veteran experienced, witnessed, or was confronted with an event or circumstance that involved actual or threatened death or serious injury, or a threat to the physical integrity of the veteran or others, such as from an actual or potential improvised explosive device; vehicle-imbedded explosive device; incoming artillery, rocket, or mortar fire; grenade; small arms fire, including suspected sniper fire; or attack upon friendly military aircraft, and the veteran’s response to the event or circumstance involved a psychological or psycho-physiological state of fear, helplessness, or horror.
Once you’ve established the stressors that qualify you for a PTSD diagnosis and you receive a service connection, the VA will determine your level of disability using your documentation and C&P exam, and award benefits accordingly.
Also see the VA page “VA disability compensation for PTSD.”
What does PTSD VA disability pay?
Your PTSD rating will compensate you based on your total disability rating. The disability rating you’re given for PTSD is combined with any other disability ratings you have, if any, to give you an overall rating based on VA math.
There is no “PTSD rate” for VA disability compensation; the disability rating at any given percentage pays based on that percentage (e.g, 50%, 70%, 90%) no matter what condition(s) gave you that rating.
To check the current year’s VA disability rates, you look at the VA’s benefits page, or check out our post on How Much Is VA Disability for 2021 compensation rates. We discuss rates for 2002 at this post: 2022 Military Disability Pay Chart
Can I work with a PTSD VA rating?
Yes, you can still work with a 100 percent schedular PTSD rating. You can work with any VA schedular rating; however, with Total Disability Individual Unemployability, or TDIU (s a rating for veterans who can’t work due to their service-connected disability) there are income restrictions, even though you can still work. (For more on TDIU,
Veterans with a 100 VA disability from the VA for PTSD also qualify for Special Monthly Compensation, which is a higher rate of compensation that the VA pays to veterans with certain needs or disabilities (and potentially spouses, surviving spouses, and parents).
How can I help a veteran with PTSD?
One way to help is by encouraging veterans to seek counseling or treatment.
One of the first and most difficult tasks in treating a veteran with PTSD is getting the veteran to acknowledge there’s a mental health condition in the first place.
Veterans (and active military personnel) are often reluctant to seek care for mental health concerns for many reasons, including the perception that it’s a sign of weakness, fear of potential career repercussions, mistrust of medicine and skepticism about treatment.
Also, many former service members and their loved ones don’t know how to identify PTSD or seek treatment. Because PTSD can be hidden, it can be difficult for health practitioners and other individuals to gauge its severity.
Additionally, PTSD in veterans is often misunderstood to be a condition that only affects combat veterans or those who have firsthand experience of violence. For VA rating purposes, the veteran must personally have experience or witnessed the stressor event firsthand.
There are many resources to turn to in order to encourage veterans to seek help or for family and friends to get educated. Here is a partial list:
A campaign creating ways for veterans and their family members to connect with the experiences of other veterans—and ultimately to connect with information and resources.
National Alliance on Mental Illness (NAMI) HelpLine
The NAMI HelpLine is a free, nationwide peer-support service providing information, resource referrals and support to people living with a mental health condition, their family members and caregivers, mental health providers and the public.
VA.gov’s Coaching Into Care
A national telephone service of the U.S. Dept. of Veterans Affairs (VA) which aims to educate, support, and empower family members and friends who are seeking care or services for a veteran. To speak with a VA coach, call 888-823-7458, Monday through Friday, 8:00 a.m. to 8:00 p.m. ET.
Veterans Crisis Line
- Call 1-800-273-8255 (Press 1)
- Text to 838255.
- Chat confidentially now.
The Mission Continues
An organization that provides veterans leadership and advocacy opportunities in their local communities, helping give former service members a sense of purpose and aiding them in the transition to civilian life.
Outward Bound’s Veteran’s Program
Outward bound provides wilderness courses and programs to build leadership and confidence among participants, and offers a specialized program for veterans.
Support groups can help veterans by providing them with a community of colleagues who have had similar experiences.
The VA provides a helpful resource on how to start a support group for veterans. There may be additional support groups available from veteran, religious, nonprofit and health organizations in the veteran’s community
Additionally, veterans can also join digital communities on platforms such as Facebook, where they can share experiences with veterans across the world who may be suffering from similar illnesses.
How can I obtain a Service Dog for PTSD?
The Americans with Disabilities Act (ADA) defines service animals as dogs that are individually trained to perform tasks for the benefit of an individual with a disability. This can be a physical, sensory, psychiatric, intellectual, or other mental disability.
To qualify for a service animal, all you need to do is get written documentation from your healthcare provider that you have and are being treated for an emotional or psychiatric disorder or disability, and require the assistance of an animal because of it.
The work a dog has been trained to do must specifically relate to your condition.
A psychiatric service dog (PSD) is a specific type of service animal trained to assist those with mental illnesses. These include post-traumatic stress disorder (PTSD). For example, a dog may assist someone with PTSD in doing room searches or turning on lights. Or it might help someone in a dissociative episode from wandering into danger. Although providing companionship and a sense of safety or calming anxiety are also important to many veterans, they’re not legally considered “tasks.”
If the dog is going to assist you in tasks you wouldn’t otherwise be able to do, you’ll probably need a service animal, which is a more highly trained dog that can be harder to obtain. If the goal is companionship, non-judgmental positive regard, and affection, an emotional support animal (ESA) or therapy animal may be a better fit and is generally easier to obtain.
A number of nonprofits train service dogs and emotional support dogs for veterans specifically and offer them to veterans who need them at no charge. Here are a few to explore:
Service Dogs Helping Veterans with PTSD
Can I buy a gun with a PTSD VA rating?
Some veterans are afraid to pursue a PTSD claim, or any other mental health claim, because of concern that they will no longer be allowed to own guns.
There are prohibitions against owning a gun under certain conditions as laid forth in VA Title 18 U.S.C. § 922, such as that the applicant “has not been adjudicated as a mental defective or been committed to a mental institution,” but there is no direct prohibition against firearm ownership simply on the grounds of having a mental health diagnosis.
In real terms, that translates as being an imminent threat to yourself or others, or having been committed to a psychiatric facility by law enforcement due to threatening behavior or signs of mental illness.
Further, the VA does not automatically report veterans who apply for disability benefits based on a mental health diagnosis, and no particular PTSD or other mental health rating prohibits a veteran from purchasing or owning firearms.
The overwhelming majority of people rated for PTSD can legally own guns.
We’ve helped many thousands of veterans obtain or increase a VA disability rating for PTSD.
While many organizations consider PTSD a complicated rating to obtain, we believe that when you know how to build your claim correctly it’s among the top three easiest claims to win. Our veteran coaches are trained and experienced in working with these kinds of claims.
Reach out to us for a FREE VA Claim Discovery Call about your PTSD claim.
Also check out these supportive related educational articles:
How To File A VA Claims for PTSD
Six Common PTSD Misconceptions
Six Tips About the PTSD Rating Scale
How To Get 100% VA Disability for PTSD
Top Five Tips to Increase your VA Disability Rating for PTSD
MAKE SURE YOU GET ALL THE BENEFITS YOU DESERVE
Most veterans are underrated for their disabilities and therefore not getting the compensation they deserve. At VA Claims Insider, we help veterans understand and take control of the claims process so they can get the rating and compensation they’re owed by law.
Our process takes the guesswork out of filing a VA disability claim and supports you every step of the way in building a fully-developed claim (FDC)—so you can increase your rating in less time!
If you’ve filed your VA disability claim and have been denied or have received a low rating – or you’re not sure how to get started, reach out to us for a FREE VA Claim Discovery Call—so you can FINALLY get the disability rating and compensation you deserve. We’ve supported more than 25,000 veterans to win their claims. NOW IT’S YOUR TURN.
ABOUT THE AUTHOR

Coach Rylan Reilkoff
Rylan enlisted at 19 years old into the US Air Force and served from 1998-2002. His father had served 22 years in the US Navy and his grandfather was in the Royal Canadian Navy. Rylan himself always wanted to serve!
While in the Air Force, his occupation was a Dietary Technician.
After leaving the US Air Force, Rylan spent 13+ years in hotel sales. He understands how to successfully move clients through a process from start to finish. He recognizes the importance of attention to detail and follow-up, which helps build trust with clients. Having worked with multiple sales teams in multiple cities and states also helps Rylan develop long-lasting relationships with clients.
Rylan says, “As a coach and former Air Force Veteran, my goal is to help as many fellow veterans navigate through the VA process and give everyone the assistance they need to get what they legally and morally deserve from the VA.“