Looking for Expert-Level VA Claim Answers?📱Call Us Now! 737-295-2226
Nerve damage is a huge concern for millions of veterans. In fact, over two million veterans suffer from nerve damage. Nerve damage can be difficult to deal with and often leads to a decrease in quality of life. A VA rating for nerve damage can help veterans get the care and compensation they deserve.
If you’re a veteran dealing with nerve damage, read on to learn more about how you can earn a VA disability rating for nerve damage.
Table of Contents

What is Nerve Damage and How Does it Happen?
When you hear the term “nerve damage,” you might think of an injury to a nerve in your arm or leg. However, nerve damage can occur anywhere in the body, and it can have a variety of causes.
Nerve damage can be caused by physical trauma, exposure to toxins or chemicals, or certain medical conditions, including cancer, diabetes, and other infectious diseases.
When nerve damage occurs, it can result in pain, numbness, or weakness in the affected area. Nerve damage can be temporary or permanent, and it can range from mild to severe.
Types of Nerve Damage
Your peripheral nerves are the nerves that relay information from your brain to the rest of your body. They’re the nerves outside of your brain and spinal cord.
When you’re assigned a VA disability rating for nerve damage throughout your body, the VA typically refers to the disability as a type of peripheral neuropathy. Neuropathy is a word associated with damage to your peripheral nerves. For the remainder of this article, we’ll refer to peripheral neuropathy as nerve damage.
Different nerves throughout your body are responsible for different functions. Since your peripheral nerves have different functions, the symptoms associated with nerve damage depend on the type of nerves affected. Your body’s nerves are classified into three different categories, including:
- Sensory nerves, or the nerves that send information to your brain. Sensory nerves control what you feel, including pain, temperature, or light touch.
- Motor nerves, or the nerves that control your motor function and body movement.
- Autonomic nerves, or the nerves that regulate your body’s core functions. Examples include breathing, blood pressure, heart rate, digestion, and bladder function.
While nerve damage can impact your entire body, most veterans suffering from nerve damage usually experience weakness, numbness and pain—most commonly in their hands, feet, and back. Depending on the type of nerve damage, other body functions like digestion, urination, and circulation can be affected.
Below, we break down common symptoms by the three types of nerves.
Nerve damage symptoms include:
Sensory nerves
- Numbness
- Tingling
- Sensitivity
- Pain
- Loss of feeling in body parts
- Loss of balance from losing feeling in body parts
- Changes to the way you walk
Motor nerves
- Muscle weakness
- Muscle twitching
- Trouble eating or swallowing
- Paralysis
- Cramps
- Loss of muscle or bone
Autonomic nerves
- Too much or not enough sweating to regulate body heat
- Changes in skin, nails, or hair
- Loss of bladder control
- Diarrhea, constipation, or incontinence
- Sexual dysfunction
- Dizziness or fainting from loss of control over blood pressure
- Irregular heartbeat
- Difficulty breathing
In order to diagnose nerve damage, your doctor may perform a range of neurological tests to determine the location and severity of your nerve damage. These tests could include blood tests, spinal fluid tests, muscle strength tests, tests of your ability to detect vibrations, CT scans, MRI scans, and nerve and skin biopsies.
How Do I Get My Nerve Damage Condition Service-Connected by the VA?
To be eligible for compensation for a VA rating for nerve damage, you must prove that your condition resulted from your military service. The VA also calls this service connection.
The VA has three requirements to prove your nerve damage is service-connected. You must:
- Have a current medical diagnosis of nerve damage.
- Have an event, injury, or diagnosis that happened while you were serving.
- Have a link, or nexus, that connects your nerve damage diagnosis to your in-service event, injury, or diagnosis.
Presumptive Nerve Damage
If you’re experiencing nerve damage symptoms that resulted from certain exposures or conditions that the VA presumes to be connected to nerve damage, you won’t be required to prove a medical nexus between your condition and your military service. These conditions include:
Herbicides
If you were exposed to herbicides such as Agent Orange during your service and develop early-onset nerve damage symptoms that are at least 10% disabling within one year of your discharge, you could be eligible for presumptive service connection.
Autoimmune Diseases
If you’re already diagnosed with certain autoimmune diseases, you could be eligible to receive a VA rating with a secondary claim for nerve damage. Conditions such as multiple sclerosis or lupus are known to cause nerve damage, and can be granted presumptive service connection if certain conditions are met and you have primary service connection for the autoimmune condition.
How does presumptive service connection work?
The VA presumes that certain conditions are caused by military service. Examples of presumptive conditions include veteran exposure to Agent Orange, burn pit exposure, or Gulf War-related disabilities.
When there’s accumulated evidence of repeated associations between specific medical conditions and specific service environments, the VA presumes that these links are not coincidental and that the disability was caused by military service. The VA created the VA Presumptive List to address this and make it easier for affected veterans to pursue their disability claims and receive benefits.
A presumptive service connection only satisfies the requirement to prove the link or medical nexus. Instead, the VA assumes the link, or nexus. (The other claim requirements still apply.)
VA-Ratable Nerves
Here are the nerves that the VA rates for nerve damage:
- The radial nerve – runs down your arm from your armpit and helps you move your elbow, wrist, hand, and fingers.
- The median nerve – gives sensation to your forearm and parts of your hand. It also helps you move your forearm, wrist, hand, and fingers.
- The ulnar nerve – runs from your neck down into your hand and helps control movement and sensation in your forearm, hand, and ring and pinky fingers.
- The musculocutaneous nerve – runs down your arm and gives sensation to your forearm and elbow; also helps move the muscles in your arm.
- The circumflex nerve – travels from the radial nerve through your shoulder, chest, and back. It’s responsible for skin sensation.
- The long thoracic nerve – extends from your shoulder down into your arm but also affects your chest. It gives sensation and movement to your shoulder and controls the muscles near your rib cage.
- The sciatic nerve – the largest nerve extending from the lower back down into each leg. This is one of the most common service-connected conditions for veterans. Read more in this post about getting a VA rating for sciatica.
- The common peroneal nerve – branches from the sciatic nerve and gives movement and sensation to your lower leg, foot, and toes.
- The superficial peroneal nerve – controls the ability to bend or flex your feet upward at the ankle.
- The tibial nerve – gives motor function to your feet and sensation in your heels.
- The anterior crural nerve (femoral) – gives motor function and sensation to your thighs.
- The internal saphenous nerve – runs throughout your legs and when damaged can impact your knees.
- The obturator nerve – controls sensation and movement in your inner thighs.
- The external cutaneous nerve of the thigh – controls sensation on the sides of your thighs.
- The ilio-inguinal nerve – controls sensation in the groin area.
How the VA Rates Nerve Damage
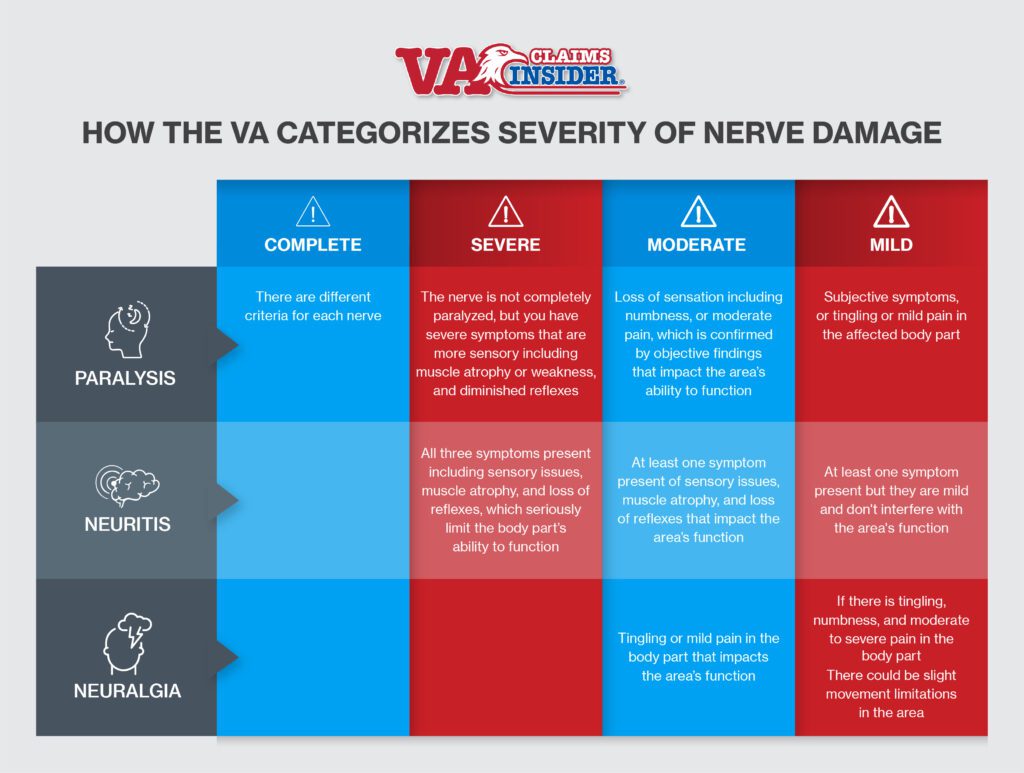
The VA rates nerve damage to each of the nerves below under three separate categories: paralysis, neuritis, and neuralgia.
When rating your nerve damage, the VA will decide which category your nerve damage falls under.
Each peripheral nerve has a different diagnostic code in each of the three categories. (Diagnostic codes are simply how the VA categorizes your disability.) There is no single diagnostic code for nerve damage. In fact, there are 70 different diagnostic codes for peripheral nerve damage.
After deciding which category your nerve damage falls into, the VA will then decide the level of severity under that category. Finally, the VA will look at the symptoms and assign a rating based on your symptoms.
Your nerve damage may be eligible under more than one diagnostic code, so understanding which code gives you the highest rating will help you get the highest rating possible.
First, let’s dive into each of the three categories of nerve damage.
Paralysis
Paralysis is the most severe category of the three and can result in the highest VA rating. To be rated for paralysis, the affected nerve must have partial or complete paralysis. The VA rates paralysis from nerve damage on a scale from mild to complete.
In order to get a “severe” rating or higher, you must have symptoms that extend beyond sensory symptoms into motor control. If you’re only experiencing numbness and tingling, the highest rating you’re eligible for is moderate.
Also, in order to get a complete paralysis rating, the body part must be completely paralyzed, not just the nerve itself.
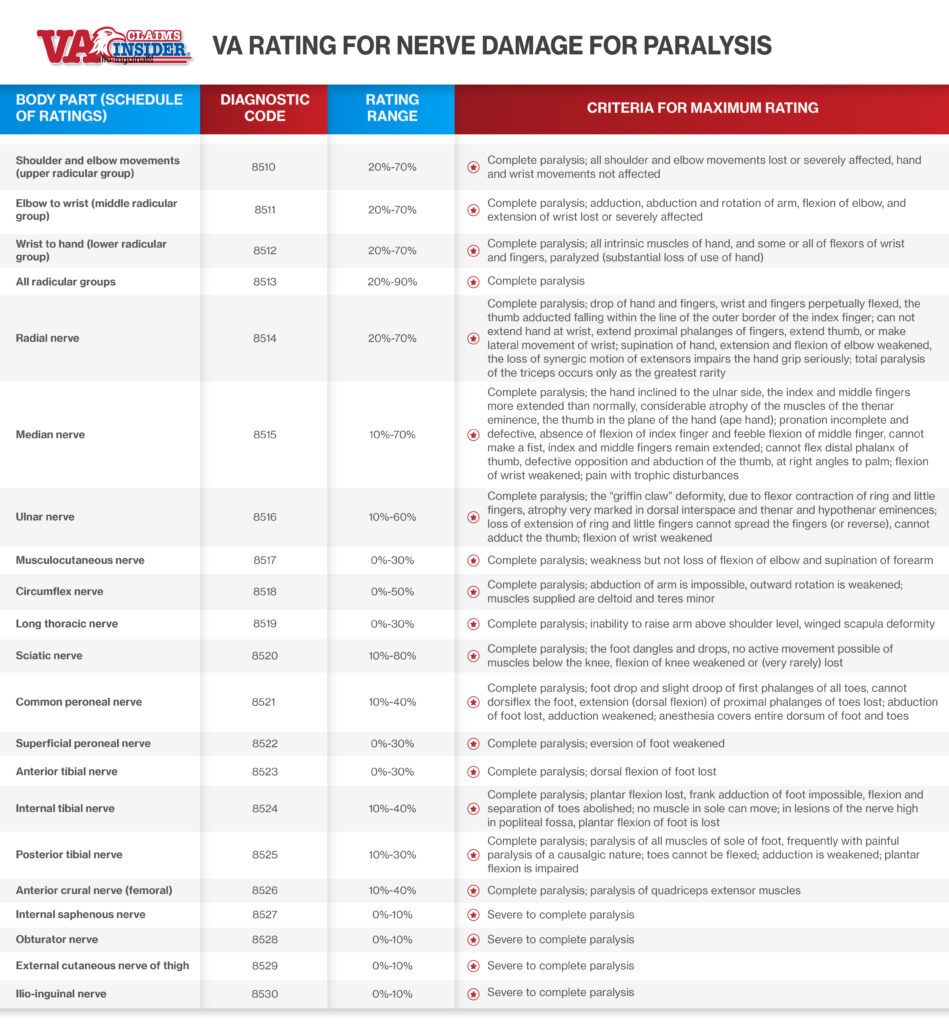
Below, we show you the rating range for paralysis of each peripheral nerve, and the requirement to get the highest VA rating for nerve damage.
VA Rating for Nerve Damage for Paralysis
Neuritis
Neuritis is defined as inflammation of the nerves. The symptoms of neuritis vary depending on the affected nerve(s), and neuritis is not always painful.
You must have at least one of these symptoms: tingling and numbness, muscle atrophy, or loss of reflexes. The VA rates neuritis from mild to severe. You can get a VA rating for nerve damage for severe neuritis up to 70%, depending on the nerve affected.
Neuralgia
Neuralgia also involves irritated or damaged nerves. Neuralgia refers to the sharp, stabbing, or burning pain that follows the path of a damaged or irritated nerve. It’s possible to experience neuralgia as a result of neuritis.
Neuralgia cannot be rated higher than moderate, even if it is considered severe. If the condition is moderate, it’s usually rated up to 20%. It can be rated up to 40% if entire limbs are affected.
The VA rates nerve damage on a scale from mild to complete. Your rating will depend on where you fall within that scale.
Additional Considerations for Nerve Damage
What’s included in your C&P Exam for nerve damage?
You’ll attend a compensation and pension (C&P) exam in order to receive a VA rating for nerve damage. The examiner will use a form called the Peripheral Nerves Conditions Disability Benefits Questionnaire to help the VA assign you a rating.
Understanding what’s on this form before the exam will help you adequately prepare for and describe your symptoms during the exam, and improve your chances of receiving a higher rating.
This questionnaire asks for:
- Relevant medical records or service treatment records
- Diagnosis of your peripheral nerve condition
- A history of your peripheral nerve condition
- The symptoms you experience—ranked as mild, moderate, or severe—for:
- Constant pain, intermittent pain, parasthesias/dysethesias, and numbness
- Each limb
- Muscle strength testing rated from normal strength to no muscle movement for:
- Elbow flexion and extension
- Wrist flexion and extension
- Grip
- Pinch (thumb to index finger)
- Knee extension
- Ankle flexion and dorsiflexion
- Whether or not you have muscle atrophy and where, with measurements
- A deep tendon reflex exam
- A sensory exam testing sensation for light touch
- Abnormalities in the skin or tissue including
- Changes in how the hair grows
- Changes in your nails
- Skin changes
- If your gait is normal or not, and a description of how it’s abnormal, if relevant
- Special tests for median nerve (in your arm)
The Bilateral Factor Can Increase Your VA Rating by an Additional 10%
The VA has a special consideration called the bilateral factor that affects your VA rating for nerve damage. The VA pairs your arms, legs, and certain skeletal muscles. If your disabilities affects both arms or both legs, the VA will rate you differently (higher) than if it affects only one of these limbs.
Following the standard VA rating procedure, you’ll receive a separate rating for each side. These two ratings will be combined, but then an additional 10% will be added on before being combined with any other disability ratings.
This is because the VA recognizes that you may be able to do far less when both your arms or legs are affected by one or multiple disabilities. NOTE: you can have different disabilities on each side of the pair to still be eligible for the bilateral factor.

NEED MORE ASSISTANCE?
Most veterans are underrated for their disabilities and therefore not getting the compensation they’re due. At VA Claims Insider, we help you understand and take control of the claims process, so you can get the rating and compensation you’re owed by law.
Our process takes the guesswork out of filing a VA disability claim and supports you every step of the way in building a fully developed claim (FDC)!
If you’ve filed your VA disability claim and have been denied or have received a low rating—or you’re unsure how to get started—reach out to us! Take advantage of a VA Claim Discovery Call. Learn what you’ve been missing—so you can FINALLY get the disability rating and compensation you deserve!
We’ve supported more than 25,000 veterans to win their claims and increase their ratings. NOW IT’S YOUR TURN.
About the Author

Brian Reese
Brian Reese is a world-renowned VA disability benefits expert and the #1 bestselling author of VA Claim Secrets and You Deserve It. Motivated by his own frustration with the VA claim process, Brian founded VA Claims Insider to help disabled veterans secure their VA disability compensation faster, regardless of their past struggles with the VA. Since 2013, he has positively impacted the lives of over 10 million military, veterans, and their families.
A former active-duty Air Force officer, Brian has extensive experience leading diverse teams in challenging international environments, including a combat tour in Afghanistan in 2011 supporting Operation ENDURING FREEDOM.
Brian is a Distinguished Graduate of Management from the United States Air Force Academy and earned his MBA from Oklahoma State University’s Spears School of Business, where he was a National Honor Scholar, ranking in the top 1% of his class.