Looking for Expert-Level VA Claim Answers?📱Call Us Now! 737-295-2226
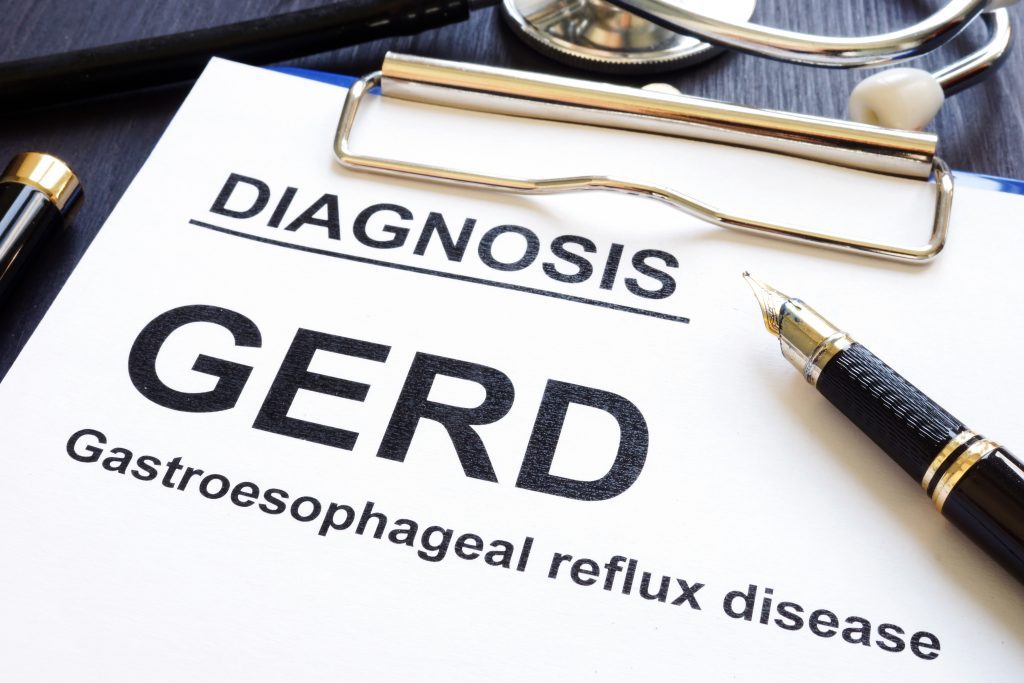
Today, you’ll learn about the 10 most common VA secondary conditions to GERD.
We also took the time to explain each one in-detail along with the appropriate VA rating criteria, medical research studies, and BVA case history to help you prove secondary service connection for GERD.
We’ve got a lot to cover, so let’s begin!
- What are VA Secondary Conditions?
- Need a Nexus Letter to Help Establish Secondary Service Connection for GERD?
- 10 Most Likely VA Secondary Conditions to GERD
- What Conditions are Secondary to GERD?
- #1. GERD Secondary to Asthma
- #2. GERD Secondary to Medications
- #3. GERD Secondary to Anxiety
- #4. GERD Secondary to Depression
- #5. GERD Secondary to PTSD
- #6. GERD Secondary to Weight Gain Obesity as Interim Link
- #7. Asthma Secondary to GERD
- #8. Migraines Secondary to GERD
- #9. Sleep Apnea Secondary to GERD
- #10. Esophagitis and Barrett’s Esophagus Secondary to GERD
- Tired of Fighting the VA Alone? WE CAN HELP!
- About the Author
What are VA Secondary Conditions?

In accordance with 38 CFR § 3.310 disabilities that are proximately due to, or aggravated by, service-connected disease or injury, a current disability condition, which is proximately due to or the result of a service-connected disease or injury shall be service connected.
Service connection on a secondary basis requires a “showing of causation.”
A showing of causation requires that the secondary VA disability claim is “proximately due to” or “aggravated by” another service-connected disability.
There are three key elements that must be satisfied to prove VA secondary service connection under the law:
- A medical diagnosis of the secondary VA disability you’re attempting to link to the current service connected disability (must be documented in a medical record) AND
- A current service-connected primary disability (e.g., your current list of service connected disabilities from your VA.gov account) AND
- Medical nexus evidence establishing a connection between the service-connected primary condition AND the current disability you’re trying to connect secondary (e.g., Migraines, Sleep Apnea, GERD, IBS, Erectile Disfunction / Female Sexual Arousal Disorder, Radiculopathy, etc.)
The FIRST part can be satisfied with any existing medical evidence in service treatment records, VA medical records, or any private medical records.
The SECOND part can be satisfied with a veteran’s existing service-connected disability rated at 0% or higher.
The THIRD part, and often the missing link needed to establish secondary service connection, can be satisfied with a credible Nexus Letter (Independent Medical Opinion) from a private healthcare provider.
Need a Nexus Letter to Help Establish Secondary Service Connection for GERD?
Click HERE now to join VA Claims Insider Elite, our premier education-based membership program, which also gets you discounted access to independent medical providers in our referral network for medical examinations, VA disability evaluations, and credible Nexus Letters for a wide range of conditions!
VA Claims Insider is the #1 most trusted name in VA claims and is a company OF veterans, BY veterans, FOR veterans.
We Help Veterans Get the VA Rating They Deserve Faster (Even If You’ve Already Filed, Been Denied, Gave Up, or Don’t Know Where to Start!)
10 Most Likely VA Secondary Conditions to GERD

- #1. GERD Secondary to Asthma
- #2. GERD Secondary to Medications
- #3. GERD Secondary to Anxiety
- #4. GERD Secondary to Depression
- #5. GERD Secondary to PTSD
- #6. GERD Secondary to Weight Gain Obesity as Interim Link
- #7. Asthma Secondary GERD
- #8. Migraines Secondary to GERD
- #9 Sleep Apnea Secondary to GERD
- #10. Esophagitis and Barrett’s Esophagus Secondary to GERD
What Conditions are Secondary to GERD?
#1. GERD Secondary to Asthma
According to the Mayo Clinic, acid reflux and Asthma often occur together. It isn’t clear why, but it’s known that acid reflux can worsen asthma and asthma can worsen acid reflux, especially severe acid reflux, a condition known as Gastroesophageal Reflux Disease (GERD).
A theory postulates that bronchospasm may cause GERD. Another theory is that medicines used to treat asthma may cause GERD. For instance, systemic steroids are known to cause reflux. An older asthma medicine, one sometimes still used for difficult to treat asthma, is theophylline. It works similar to caffeine and may relax the esophageal sphincter. Bronchodilaors like albuterol may also cause the esophageal sphincter to relax, resulting in GERD. Another medicine that is commonly used to treat asthma, beta-adrenergic bronchodilators, may aggravate acid reflux.
Can GERD be a secondary VA claim to Asthma?
Yes, GERD can be service-connected secondary to Asthma.
The VA Ratings for GERD secondary to Asthma are 10%, 30%, or 60% depending upon the severity of your GERD, and how your GERD symptoms affect your work, life, and social functioning. It also depends upon the frequency and duration of your symptoms, meaning, the more severe your symptoms, the higher the VA rating for GERD.
For example, a veteran may only have a 10% rating for Asthma but could possibly receive a 30% or 60% VA rating (lower rating possible as well) for GERD secondary to Asthma.
VA Disability Ratings for GERD Explained:
Medical Research Studies:
Review article: gastro-esophageal reflux disease in asthma and chronic obstructive pulmonary disease
Asthma, GERD and Obesity: Triangle of Inflammation
BVA Case History Example:
GERD Secondary to Asthma is Granted
#2. GERD Secondary to Medications
GERD can develop when the symptoms of mental health conditions, such as anxiety, stress, and depression, lead to an overproduction of stomach acid. In some people, medications taken to treat PTSD and other mental health conditions can lead to GERD (acid reflux) as a side effect.
A study claimed that Gastroesophageal reflux disease (GERD), which is common in many communities, is associated with structural factors, eating habits, and the use of certain medications. The use of such medications (whether over the count or prescribed) can lead to the emergence of GERD and can also exacerbate existing reflux symptoms. These drugs can contribute to GERD by directly causing mucosal damage, by reducing lower esophageal sphincter pressure (LESP), or by affecting esophagogastric motility.
Can GERD be a secondary VA claim to Medication Side Effects?
Yes, GERD can be service-connected secondary to Medication Side Effects as an “Interim Link” to another service connected condition.
The VA Ratings for GERD secondary to Medication Side Effects are 10%, 30%, or 60% depending upon the severity of your GERD, and how your GERD symptoms affect your work, life, and social functioning. It also depends upon the frequency and duration of your symptoms, meaning, the more severe your symptoms, the higher the VA rating for GERD.
While Medication Side Effects are not a ratable VA disability on its own, Medication Side Effects may be used as an “Interim Link” for secondary service connection. How? For example, if a veteran takes medications to manage symptoms of a service connected disability (PTSD in this example) and those medications cause side effects of a (new) non service connected disability, the new disability can be connected as a secondary VA claim to the service connected condition with Medication Side Effects as the Interim Link. The best example would be a veteran who is taking antidepressants to manage symptoms of PTSD, and those antidepressants have side effects leading to GERD (acid reflux). Thus, while the PTSD might not necessarily “cause” the GERD, the side effects of the medications taken to manage PTSD symptoms can be used as the “Interim Link” for service connecting GERD secondary to PTSD.
VA Disability Ratings for GERD Explained:
Medical Research Study:
Which drugs are risk factors for the development of gastroesophageal reflux disease?
BVA Case History Example:
GERD Secondary to Medication Side Effects is granted
#3. GERD Secondary to Anxiety
GERD can develop when mental health symptoms such as anxiety, stress, and depression, among many others, lead to an overproduction of stomach acid.
According to the National Library of Medicine, Anxiety sufferers have a higher lifetime prevalence of various medical problems. Chronic medical conditions furthermore increase the likelihood of psychiatric disorders and overall dysfunction. Lifetime rates of cardiovascular, respiratory, gastrointestinal, and other medical problems are disproportionately high in anxiety and panic/fear sufferers.
The heightened comorbidity is not surprising as many symptoms of anxiety and panic/fear mimic symptoms of medical conditions.
Stress can worsen acid reflux symptoms, and anxiety is a natural response to stress in the body. Paradoxically, experiencing anxiety can also in itself be stressful, which can perpetuate the acid reflux cycle.
There is some evidence to suggest that stress and anxiety may provoke acid reflux or make the symptoms worse. For instance, a 2018 study involving more than 19,000 people found that those with anxiety were more likely to experience GERD symptoms.
Can GERD be a secondary VA claim to Anxiety?
Yes, GERD can be service-connected secondary to Anxiety.
The VA Ratings for GERD secondary to Anxiety are 10%, 30%, or 60% depending upon the severity of your GERD, and how your GERD symptoms affect your work, life, and social functioning. It also depends upon the frequency and duration of your symptoms, meaning, the more severe your symptoms, the higher the VA disability rating for GERD.
For example, a veteran may have a 50% rating for Anxiety (lower or higher rating possible as well) but could possibly receive a 10%, 30% or 60% VA rating for GERD secondary to Anxiety.
VA Disability Ratings for GERD Explained:
Medical Research Studies:
Anxiety Disorders and Medical Comorbidity: Treatment Implications
BVA Case History Example:
GERD Secondary to Anxiety is granted
#4. GERD Secondary to Depression
GERD can develop when the symptoms of anxiety, stress, and depression, among others, lead to an overproduction of stomach acid.
In a study where information about GI (Gastrointestinal) symptoms such as diarrhea, constipation, abdominal pain, and gastroesophageal reflux disease (GERD) were extracted from the clinic notes to determine if there is a relationship between PTSD and depression screenings and GI symptoms. Results state that 28% of the participants had GERD and a positive screening of depression was significantly associated with these GI symptoms.
Can GERD be a secondary VA claim to Depression?
Yes, GERD can be service-connected secondary to Depression.
The VA Ratings for GERD secondary to Depression are 10%, 30%, or 60% depending upon the severity of your GERD, and how your GERD symptoms affect your work, life, and social functioning. It also depends upon the frequency and duration of your symptoms, meaning, the more severe your symptoms, the higher the VA rating for GERD.
For example, a veteran may only have a 10% rating for Depression but could possibly receive a 30% or 60% VA rating (lower rating possible as well) for GERD secondary to Depression.
VA Disability Ratings for GERD Explained:
Medical Research Study:
BVA Case History Example:
GERD Secondary to Depression is granted
#5. GERD Secondary to PTSD
GERD can develop when the symptoms of PTSD, such as anxiety, stress, and depression, lead to an overproduction of stomach acid. In some veterans, medications taken to treat PTSD can also lead to GERD as a side effect. For further reading, please see sections in this eBook where we discuss Medication Side Effects as an “Interim Link” for secondary service connection.
In a study where information about GI (Gastrointestinal) symptoms such as diarrhea, constipation, abdominal pain, and gastroesophageal reflux disease (GERD) were extracted from the clinic notes to determine if there is a relationship between PTSD and depression screenings and GI symptoms. Results state that 28% of the participants had GERD and a positive screening of PTSD was significantly associated with these GI symptoms.
Other medical research studies support a connection between GERD and PTSD. For example, both veteran and non-veteran studies have reported high rates of comorbidity between PTSD, Depression, and Gastrointestinal (GI) symptoms.
A 2013 study of veterans who deployed to Iraq and Afghanistan found that nearly 45% of patients screened positive for PTSD and 23% screened positive for depression symptoms.
While only 11% of patients reported GI symptoms, 73.4% of these patients had a positive screen for PTSD, indicative of a significant relationship.
Many veterans with GERD or acid reflux, especially those who were diagnosed long after leaving the military are eligible under the law for GERD secondary to PTSD.
For example, if veterans are taking SSRIs to help manage their PTSD symptoms, perhaps you’re suffering from side effects of those SSRI medications, which can lead to digestive system issues.
Can GERD be a secondary VA claim to PTSD?
Yes, GERD can be service-connected secondary to PTSD.
The VA Ratings for GERD secondary to PTSD are 10%, 30%, or 60% depending upon the severity of your GERD, and how your GERD symptoms affect your work, life, and social functioning. It also depends upon the frequency and duration of your symptoms, meaning, the more severe your symptoms, the higher the VA rating for GERD.
For example, a veteran might have a 30% rating for PTSD (lower or higher rating possible for PTSD) but could possibly receive a 10%, 30% or 60% VA rating for GERD secondary to PTSD.
VA Disability Ratings for GERD Explained:
Medical Research Studies:
Post-Traumatic Stress Disorder and Gastrointestinal Disorders in the Danish Population
BVA Case History Example:
GERD Secondary to PTSD is Granted
#6. GERD Secondary to Weight Gain Obesity as Interim Link
Gastroesophageal reflux disease (GERD) is a common condition with multifactorial pathogenesis, affecting up to 40% of the population. Obesity is also common. Obesity and GERD are clearly related, both from a prevalence and causality association.
A study found that GERD symptoms increase in severity when people gain weight. Obese patients tend to have more severe erosive esophagitis and obesity is a risk factor for the development of Barrett’s esophagus and adenocarcinoma of the esophagus. Patients report improvement in GERD when they lose weight and there are several reports suggesting a decrease in GERD symptoms after bariatric surgery.
According to another study, an increase in GERD symptoms has been shown to occur in individuals who gain weight but continue to have a body mass index (BMI) in the normal range, contributing to the epidemiological evidence for a possible dose-response relationship between BMI and increasing GERD.
Can GERD be a secondary VA claim to Weight Gain Obesity as Interim Link?
Yes, GERD can be service-connected secondary to Weight Gain Obesity as Interim Link.
The VA Ratings for GERD secondary to Weight Gain Obesity as Interim Link are 10%, 30%, or 60% depending upon the severity of your GERD, and how your GERD symptoms affect your work, life, and social functioning. It also depends upon the frequency and duration of your symptoms, meaning, the more severe your symptoms, the higher the VA rating for GERD.
While a veteran can’t be rated for Weight Gain Obesity, if a service connected disability such as PTSD or Depression causes/aggravates Weight Gain Obesity, it can be used as an “Interim Link” for service connection. For example, you could possibly receive a 60% service connected VA rating for GERD secondary to Weight Gain Obesity as an Interim Link to another service connected condition, which in this example was PTSD or Depression (which you already have service connected and rated).
VA Disability Ratings for GERD Explained:
Medical Research Studies:
Gastroesophageal reflux disease and obesity
The association between obesity and GERD: a review of the epidemiological evidence
BVA Case History Example:
As of this writing, a BVA case history example could not be located. However, it’s still possible to connect the two conditions depending upon your medical evidence and medical research.
#7. Asthma Secondary to GERD
According to the Mayo Clinic, “Asthma and acid reflux often occur together. Acid reflux can worsen asthma and asthma can worsen acid reflux, especially severe acid reflux, a condition known as Gastroesophageal Reflux Disease (GERD). Asthma and acid reflux can occur together in children as well as in adults.”
Veterans with asthma are at higher risk of developing GERD. Asthma flare-ups can cause the lower esophageal sphincter to relax, allowing stomach contents to flow back, or reflux, into the esophagus. Some asthma medications, such as Theophylline may worsen reflux symptoms.
The prevalence of GERD in asthma patients has ranged from 25% to 80% in studies, many of which use self-reported GERD. In a study conducted by the American Lung Association Asthma Clinical Research Centers (ACRC) Network, 38% of asthma patients had GERD (as defined by a positive pH probe).
Acid reflux can also make asthma symptoms worse by irritating the airways and lungs, leading to progressively more serious asthma. Also, this irritation can trigger allergic reactions and make the airways more sensitive to environmental conditions such as smoke or cold air.
Can Asthma be service connected secondary to GERD?
Yes, asthma secondary to GERD is a common secondary VA claim, and it can be rated at 10%, 30%, 60%, or 100% depending upon the frequency, severity, and duration of your asthma symptoms.
Asthma is a bronchial disorder rated under CFR 38, Part 4, VA Schedule of Ratings, Diagnostic Code 6602, Asthma, Bronchial.
VA Rating for Asthma Explained:
What are the VA Disability Ratings for Asthma?
Medical Research Study:
Is There a Relationship Between GERD and Asthma?
BVA Case History Example:
Asthma Secondary to GERD Is Granted
#8. Migraines Secondary to GERD
Recent studies are increasingly linking GERD and Headaches, but some questions remain on why exactly this happens. Headaches or migraines are associated with a number of gastrointestinal conditions. These include: dyspepsia (indigestion), GERD, constipation, functional abdominal pain, inflammatory bowel syndrome (IBS), inflammatory bowel disorders (IBD), celiac disease and Heliobacter pylori (H. pylori) infection. Studies suggest that between 30 and 50 percent of people with chronic headaches or migraines also have GERD. Researchers are still trying to pinpoint which comes first, and whether GERD and headaches exist together, or if one causes the other.
Autonomic nervous system malfunction has been linked to both GERD and migraines and could contribute to the development of either — or both — conditions. Food allergies, medications, and even serotonin levels are also common threads between both headache and reflux, and could play a role in connection between the two.
Acid reflux and GERD occur when stomach acid bubbles up from the opening between the stomach and the esophagus. When the acid reaches the esophagus, it causes irritation or a burning sensation. In some cases, this backflow of stomach acids can even reach the eustachian tubes in your throat. They connect to your inner ear. The ear plays a large role in balance, and disruptions to the pressure in your ear —especially with stomach acid — can cause dizziness.
Research has also shown that people who regularly experience gastrointestinal symptoms — such as reflux, diarrhea, constipation and nausea — have a higher prevalence of headaches than do those who don’t have gastrointestinal symptoms.
Can Migraines be a secondary VA claim to GERD?
Yes, Migraines can be service-connected secondary to GERD.
The VA Ratings for Migraines secondary to GERD are 0%, 10%, 30%, or 50%, depending upon the frequency, severity, and duration of your Migraines, and how your headache symptoms affect your work, life, and social functioning.
For example, a veteran may only have a 10% rating for GERD but could possibly receive a 0%, 10%, 30%, or 50% VA rating for Migraines secondary to GERD.
VA Disability Ratings for Migraines Explained:
How Are Migraines Rated by the VA?
Medical Research Study:
Gastroesophageal Reflux Disease and Migraine Disorders
BVA Case History Example:
As of this writing, a BVA case history example could not be located. However, it’s still possible to connect the two conditions depending upon your medical evidence and medical research.
#9. Sleep Apnea Secondary to GERD
Obstructive sleep apnea hypopnea syndrome (OSAHS) means apnea and hypopnea caused by partial or complete obstruction of upper airway collapse during sleep. Gastroesophageal reflux disease (GERD) is believed to be associated with various manifestations in the otorhinolaryngology and has been found to be an additional risk factor for OSAHS. The significant correlation between obstructive sleep apnea hypopnea syndrome and gastroesophageal reflux disease has been concluded in a study posted online by National Library of Medicine.
Normal physiological adaptations of the aerodigestive system to sleep prolong and intensify nocturnal reflux events. This occurrence leads to sleep disruption, as well as to esophageal, laryngeal, and laryngopharyngeal reflux.
Can Sleep Apnea be a secondary VA claim to GERD?
Yes, Sleep Apnea can be service-connected secondary to GERD.
The VA Ratings for Sleep Apnea secondary to GERD are 0%, 30%, 50%, or 100%, depending upon the severity of your Sleep Apnea, and how your Sleep Apnea symptoms affect your work, life, and social functioning.
For example, a veteran may only have a 10% rating for GERD but could possibly receive a 30% or 50% VA rating (lower or higher rating possible as well) for Sleep Apnea secondary to GERD.
By law, there are three evidentiary elements that must be satisfied for sleep apnea secondary to GERD to prove secondary service connection:
- A medical diagnosis of sleep apnea confirmed by a sleep study in VA medical records or private records (unless you did this already on active duty and it’s in your service treatment records), AND
- Evidence of a service-connected primary disability, which in this case would be Gastroesophageal Reflux Disease (GERD), AND
- Medical Nexus evidence (Nexus Letter) establishing a link or connection between the service-connected GERD and the current Sleep Apnea.
VA Disability Ratings for Sleep Apnea Explained:
How is Sleep Apnea Rated by the VA?
Medical Research Study:
Sleep and Nocturnal Gastroesophageal Reflux: An Update
BVA Case History Example:
Sleep Apnea secondary to GERD is granted
#10. Esophagitis and Barrett’s Esophagus Secondary to GERD
GERD can cause inflammation of the esophagus, known as esophagitis. This condition involves irritation and damage to the lining of the esophagus due to acid reflux. Symptoms may include difficulty swallowing, chest pain, and heartburn. If a veteran experiences esophagitis as a direct consequence of their GERD, it can be considered a secondary condition.
Barrett’s esophagus is a more severe complication of GERD in which the lining of the esophagus undergoes changes, increasing the risk of esophageal cancer. Veterans with long-term and poorly managed GERD may develop Barrett’s esophagus. If this condition arises as a result of service-connected GERD, it can be claimed as a secondary condition.
Under 38 CFR § 4.144, Schedule of Ratings for the Digestive System, Diagnostic Code (DC) 7203, the VA may assign disability ratings for esophagitis and Barrett’s esophagus secondary to GERD at 30 percent, 50 percent, or 80 percent, depending on the severity of the condition.
DC 7203 Esophagus, stricture of:
- Permitting passage of liquids only, with marked impairment of general health rate at 80%
- Severe, permitting liquids only rate at 50%
- Moderate rate at 30%
Tired of Fighting the VA Alone? WE CAN HELP!
- VA Claims Insider is the #1 most trusted name in VA disability claims.
- 25,000+ disabled veterans served in our membership programs since 2016.
- 30% average VA rating increase for veterans who complete our #1 rated Elite program.
- Employs 215 teammates; comprised of 74 veterans and 16 military spouses.
- 4.7/5.0 average rating out of 4,500+ total reviews; over 4,000 5-star reviews.
About the Author

Brian Reese
Brian Reese is a world-renowned VA disability benefits expert and the #1 bestselling author of VA Claim Secrets and You Deserve It. Motivated by his own frustration with the VA claim process, Brian founded VA Claims Insider to help disabled veterans secure their VA disability compensation faster, regardless of their past struggles with the VA. Since 2013, he has positively impacted the lives of over 10 million military, veterans, and their families.
A former active-duty Air Force officer, Brian has extensive experience leading diverse teams in challenging international environments, including a combat tour in Afghanistan in 2011 supporting Operation ENDURING FREEDOM.
Brian is a Distinguished Graduate of Management from the United States Air Force Academy and earned his MBA from Oklahoma State University’s Spears School of Business, where he was a National Honor Scholar, ranking in the top 1% of his class.