Looking for Expert-Level VA Claim Answers?📱Call Us Now! 737-295-2226
Today, I’m revealing and explaining the Top 5 VA Secondary Conditions to Depression for VA disability benefits utilizing the legal and medical requirements for secondary service connection.
According to the Top 50 VA Disability Claims, Depression is the #14 most claimed VA disability.
While the average VA Rating for Depression is 70%, making it a high-value VA claim, did you know there are 5 OTHER high-value VA disability claims (rated at 30% or above) that can be medically linked through “aggravation” and claimed secondary to your service-connected Depression?
In our experience, many veterans don’t even realize they qualify for a variety of additional VA disability benefits due to their current service-connected Depression.
Why?
Because veterans aren’t medical experts (nor should they be), and yet, VA disability claims depend almost entirely upon MEDICAL EVIDENCE!
Depression can have significant debilitating effects on veterans, especially due to the side effects of medications taken to manage your mental health symptoms, often leading to a variety of other disabling conditions such as Migraines, Sleep Apnea, GERD, IBS, Erectile Dysfunction, and Female Sexual Arousal Disorder.
Okay, let’s jump into our Top 5 VA Secondary Conditions that are “proximately due to” or “aggravated by” service-connected Depression.
You Might Also Like the Following Blog Posts:
- The Definitive Guide to VA Ratings for Migraines
- VA Ratings for GERD: The Expert’s Guide
- How to Get a VA Disability Rating for IBS
- Top 3 Tips to Get a VA Rating for ED
How to Establish Service Connection Secondary to Depression

In accordance with 38 CFR § 3.310 disabilities that are proximately due to, or aggravated by, service-connected disease or injury, a current disability condition, which is proximately due to or the result of a service-connected disease or injury shall be service connected.
Service connection on a secondary basis requires a showing of causation.
A showing of causation requires that the secondary disability claim be shown to be “proximately due to” or “aggravated by” another service-connected disability.
There are three evidentiary elements that must be satisfied to service connect secondary conditions to Depression:
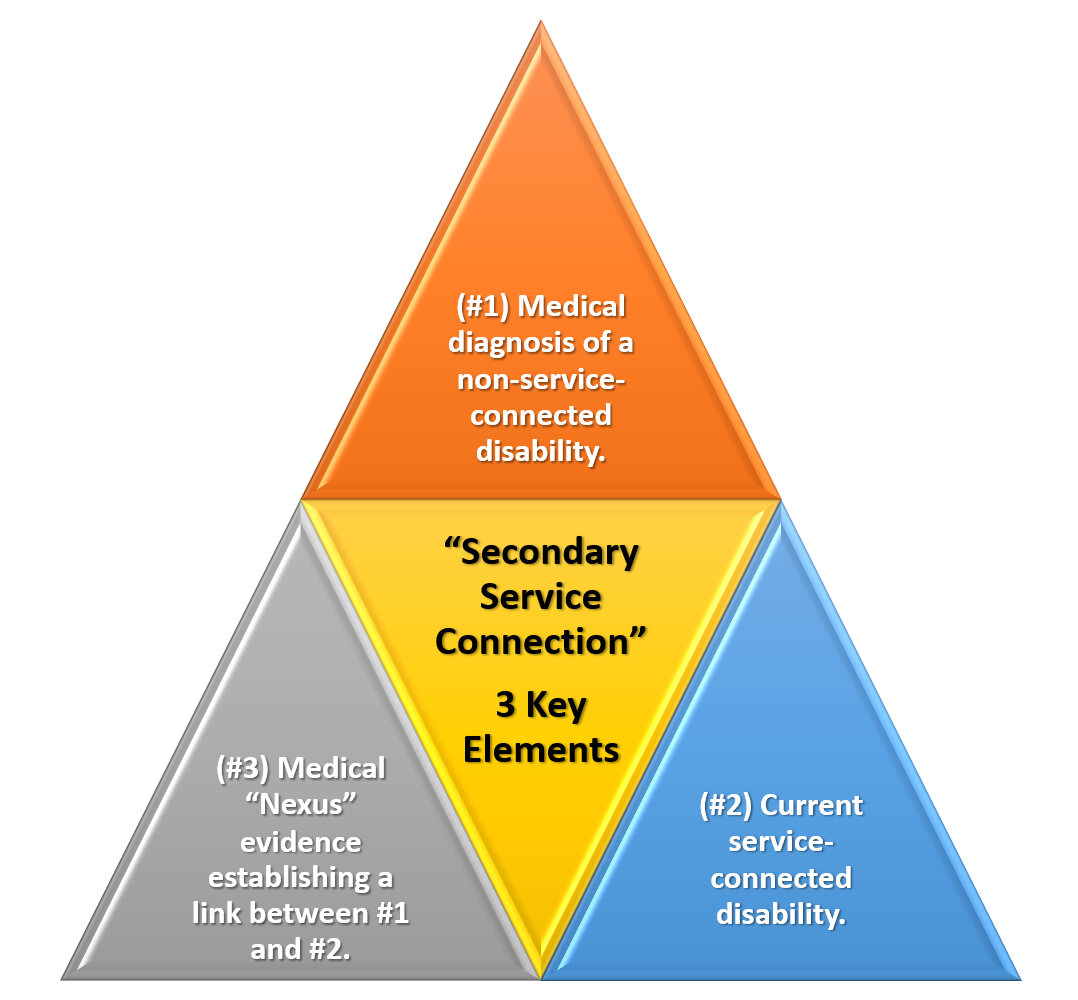
- #1. A medical diagnosis of the secondary disability condition you’re attempting to link to Depression AND
- #2. A current service-connected primary disability (e.g., your current Depression VA Rating) AND
- #3. Medical nexus evidence establishing a connection between the service-connected Depression and the current disability you’re trying to connect (e.g., Migraines, Sleep Apnea, GERD, IBS, Erectile Dysfunction / Female Sexual Arousal Disorder)
The first part can be satisfied with any existing medical evidence in service treatment records, VA medical records, or any private medical records.
The second part can be satisfied with a veteran’s existing service-connected disability rated at 0 percent or higher, which in this case, is Depression.
The third part, and often the missing link needed to establish secondary service connection, can be satisfied with a credible Nexus Letter (Independent Medical Opinion) from a qualified medical provider.
>> Wondering How to Find Doctors Who Write Nexus Letters for Veterans?
Did you know there are five primary high-value VA disability conditions that can be medically linked secondary to your current VA Depression rating?
Truth bomb here veterans…
You could be missing out on thousands of dollars of tax-free disability benefits you deserve by law, and not even realize that your current VA disability might be caused or aggravated by your service-connected Depression.
Need a Nexus Letter to help establish secondary service connection?
Click HERE Now to Join VA Claims Insider Elite, our premier education-based membership program, which also gets you discounted access to independent medical providers in our referral network for medical examinations, VA disability evaluations, DBQs, and Nexus Letters for a wide range of conditions!
Deserve a HIGHER VA Rating?
Learn more about how VA Claims Insider can help you get the rating you DESERVE!
Book a no-obligation Discovery Call today!
List of the Top 5 VA Secondary Conditions to Depression

- #1: Migraines secondary to Depression
- #2: Sleep Apnea secondary to Depression
- #3: GERD secondary to Depression
- #4: IBS secondary to Depression
- #5: ED secondary to Depression
#1. Migraines Secondary to Depression

Migraine Headaches, Tension Headaches, and Post Traumatic Headaches are the most common types of headaches in veterans although there are many others, too.
Medical research suggests a connection between Migraines and Depression.
One study found Depression affects almost 80% of those with Migraines.
Another study discovered that people with Migraines, especially chronic Migraines, are more likely to experience intense anxiety, depression, and suicidal tendencies.
The association of depression with migraine headaches is linked by a causal bi-directional relationship.
Another study found that over a two-year period, a person with a history of major depression was three times more likely than average to have a first migraine attack, and a person with a history of migraine was five times more likely than average to have a first episode of depression.
This study’s results indicated that stress and anxiety were higher in the migraine group than in the control group and above the clinical level.
In addition, they claimed that stress is a primordial factor in the triggering and perpetuation of migraine attacks.
The biological link between migraines and depression is complex and may be related to genes, low serotonin production, or other factors.
They are worth understanding more about, especially when working to manage both conditions effectively.
Scientific studies reveal that the relationship between migraine and depression is a two-way street: Having one puts you at a higher risk of the other, and worsening symptoms of one condition can also worsen the symptoms of the other, and vice versa.
Migraine headaches is one of the most common secondary conditions to Depression.
Furthermore, headaches are a common side effect of Selective Serotonin Reuptake Inhibitors (SSRIs) such as Citalopram (Celexa), Escitalopram (Lexapro), Fluoxetine (Prozac), Paroxetine (Paxil, Pexeva), and Sertraline (Zoloft).
If you’re taking medications to try to manage your Depression symptoms, but those medications cause side effects, you might be able to get service-connected secondary to Depression due to the side effects of medications and how the “cause” or “aggravate” headaches.
>> Click HERE to read my Top 6 Tips for Your VA Claim for Migraines.
You’ll likely need a Nexus Letter from an independent medical professional to establish service connection for Migraines Secondary to Depression.
Speaking of headaches, did you know there are more than 150 different types of headaches eligible for VA disability benefits under the law?
While the Schedule for Rating Disabilities only lists “Migraines,” ANY type of headache can be service connected and compensated under the law if the veteran has current symptoms of headaches that interfere with work, life, and social functioning.
What is the VA Rating for Migraines Secondary to Depression?
CFR 38, Part 4, the Schedule for Rating Disabilities, lists Migraines under code 8100.
The Migraines Secondary to Depression VA rating scale consists of four possible ratings: 0%, 10%, 30%, and 50%.
The symptoms become markedly more severe between at the 30% and 50% rating levels, as evidenced by the rating criteria below:
| Migraines Secondary to Depression VA Rating Scale: | VA Rating |
| Migraines with very frequent completely prostrating and prolonged attacks productive of severe economic inadaptability | 50% |
| Migraines with characteristic prostrating attacks occurring on an average once a month over last several months | 30% |
| Migraines with characteristic prostrating attacks averaging one in 2 months over last several months | 10% |
| Migraines with less frequent attacks | 0% |
#2. Sleep Apnea Secondary to Depression

Did you know veterans are almost four times as likely to have or develop Obstructive Sleep Apnea compared to the general population (e.g., those we did not serve in the military)?
Numerous medical research studies point to a bi-directional relationship between Sleep Apnea and Depression.
One study found that in patients with Obstructive Sleep Apnea, 53.9% of the patients had some degree of anxiety, while 46.1% demonstrated depressive symptoms.
Another study linked Obstructive Sleep Apnea with a higher prevalence of Major Depression, likely due to changes in brain chemistry caused by frequent apneic episodes (paused or stopped breathing).
The risk of Depression was significantly higher for people diagnosed with Obstructive Sleep Apnea.
In our experience, it is common for a veteran’s Depression to aggravate his/her Sleep Apnea due to Obesity as an interim link for secondary service connection.
The #1 recommendation for veterans attempting to service connect sleep apnea as a secondary condition is to get a Nexus Letter.
Why?
Because “Medical Nexus Evidence” is a required element of Secondary Service Connection!
What is the VA Rating for Sleep Apnea Secondary to Depression?
VA ratings for Sleep Apnea secondary to Depression can be rated at 0%, 10%, 30%, or 50% depending upon the severity of your sleep apnea, and how your symptoms affect your work, life, and social functioning.
For example, a veteran may have a 70% rating for Depression and then get service connected at 50% of “Sleep Apnea with CPAP” secondary to Depression.
| Sleep Apnea Secondary to Depression VA Rating Scale: | VA Rating |
| Chronic respiratory failure with carbon dioxide retention or cor pulmonale, or requires tracheostomy | 100% |
| Requires use of breathing assistance device such as continuous airway pressure (CPAP) machine | 50% |
| Persistent daytime hypersomnolence (daytime tiredness) | 30% |
| Asymptomatic but with documented sleep disorder breathing | 0% |
#3. GERD Secondary to Depression

Medical research supports a connection between GERD and Depression.
Both veteran and non-veteran studies have reported high rates of comorbidity between PTSD, Depression, and Gastrointestinal (GI) symptoms.
A 2013 study of veterans who deployed to Iraq and Afghanistan found that nearly 45% of patients screened positive for PTSD and 23% screened positive for depression symptoms.
While only 11% of patients reported GI symptoms, 73.4% of these patients had a positive screen for PTSD and Depression, indicative of a significant relationship.
A 2015 study found that anxiety and depression increase the risk of GERD, and have found that GERD’s negative effect on quality of life increases anxiety and depression, in a bi-directional relationship—the more severe the Depression, the more severe the GERD.
Many veterans with GERD or acid reflux, especially those who were diagnosed long after leaving the military are eligible under the law for GERD secondary to Depression.
For example, if veterans are taking SSRIs to help manage their symptoms of Depression, perhaps you’re suffering from side effects of those SSRI medications, which can lead to digestive system issues.
Thus, veterans can service connect GERD as a secondary condition to Depression.
What is the VA Rating for GERD Secondary to Depression?
GERD secondary to Depression is a VA disability and can be rated at 10%, 30%, or 60%, depending upon the frequency, severity, and duration of symptoms.
GERD is typically rated analogous to Hiatal Hernia under CFR 38, Part 4, VA Schedule of Ratings, Diagnostic Code 7346, Hernia Hiatal.
| GERD Secondary to Depression VA Rating Scale: | VA Rating |
| GERD with symptoms of pain, vomiting, material weight loss and hematemesis or melena with moderate anemia; or other symptom combinations productive of severe impairment of health | 60% |
| GERD with persistently recurrent epigastric distress with dysphagia, pyrosis, and regurgitation, accompanied by substernal or arm or shoulder pain, productive of considerable impairment of health | 30% |
| GERD with two or more of the symptoms for the 30 percent evaluation of less severity | 10% |
#4. IBS Secondary to Depression

Medical research points to a connection between IBS and Depression.
Both physiologic and psychosocial variables appear to play important roles in the development and maintenance of IBS.
Recent information suggests that the association of IBS and psychiatric disorders may be more fundamental than was previously believed and a significant amount of clinical and research data suggest the importance of the brain-gut interaction in IBS.
In a study published by the National Library of Medicine, they examined the observed high prevalence of psychiatric disorders in patients with IBS.
The published literature indicates that fewer than half of individuals with IBS seek treatment for it.
Of those who do, 50% to 90% have psychiatric disorders, including panic disorder, generalized anxiety disorder, social phobia, posttraumatic stress disorder, and major depression, while those who do not seek treatment tend to be psychologically normal.
Veterans should read this BVA decision from 2016, where a veteran was granted secondary service connection for IBS, which was proximately due to or the result of medication side effects taken to manage symptoms of other service-connected disabilities:
“There is an approximate balance of favorable and unfavorable evidence as to whether the Veteran has irritable bowel syndrome proximately due to or the result of pain medications from his service-connected hiatal hernia, thoracolumbar spine, cervical spine, migraine headache, bilateral hip, bilateral shoulder, and bilateral knee disabilities. Resolving all reasonable doubt in his favor (aka, Benefit of the Doubt Doctrine “Tie goes to the runner,”) the Veteran has irritable bowel syndrome secondary to medication from his service-connected disabilities. See 38 U.S.C.A. 1110, 5103, 5103A, 5107 (West 2014); 38 CFR 3.102, 3.159, and 3.310.”
– BVA Case Decision DOCKET NO. 06-05 255
What is the VA Rating for IBS Secondary to Depression?
VA ratings for IBS secondary to Depression are either 0%, 10%, or 30%.
IBS is a digestive system issue and is most often rated under CFR 38, Part 4, VA Schedule of Ratings, Diagnostic Code 7319, Irritable Colon Syndrome.
| IBS Secondary to Depression VA Rating Scale: | VA Rating |
| IBS severe; diarrhea, or alternating diarrhea and constipation, with constant abdominal distress | 30% |
| IBS moderate; frequent episodes of bowel disturbance with abdominal distress | 10% |
| IBS mild; disturbances of bowel function with occasional episodes of abdominal distress | 0% |
#5. ED Secondary to Depression

Medical research points to a strong connection between Erectile Dysfunction (ED) and Depression.
Although urologists and psychiatrists have long recognized that antidepressant medications affect erectile function negatively, the interplay between the two conditions remains underappreciated.
One study found that in patients with mild-to-moderate grades of depression, sexual dysfunction was seen in 62.5% of the patient group.
Significant differences were seen with decreased sexual desire, orgasmic problems, and overall dissatisfaction in the patient group.
Thus, Depression was found to be significantly associated with sexual functioning (erective dysfunction in men and female sexual arousal disorder in women).
Low testosterone, also known as “low T,” is common in men with mental health issues like depression and anxiety who experience erectile dysfunction.
According to another research study on the relationship between ED and Depression:
- 47% of people with depression have unhealthy sex lives.
- 61% of people with severe depression have some sort of sexual problem.
- 40% of them end up taking antidepressants which may also affect their sexual lives.
- 80%+ of men with erectile dysfunction have had depression at some point in their lives.
What is the VA Rating for ED Secondary to Depression?
Most veterans will receive a 0% non-compensable rating for ED secondary to Depression.
Service connection for ED secondary to Depression makes veterans eligible for Special Monthly Compensation (SMC)-K for the loss of use of a creative organ.
The current SMC-K rate for 2022 is $118.33 per month, which is paid in addition to a veteran’s regular (schedular) service connected disability compensation.
About the Author

Brian Reese
Brian Reese is a world-renowned VA disability benefits expert and the #1 bestselling author of VA Claim Secrets and You Deserve It. Motivated by his own frustration with the VA claim process, Brian founded VA Claims Insider to help disabled veterans secure their VA disability compensation faster, regardless of their past struggles with the VA. Since 2013, he has positively impacted the lives of over 10 million military, veterans, and their families.
A former active-duty Air Force officer, Brian has extensive experience leading diverse teams in challenging international environments, including a combat tour in Afghanistan in 2011 supporting Operation ENDURING FREEDOM.
Brian is a Distinguished Graduate of Management from the United States Air Force Academy and earned his MBA from Oklahoma State University’s Spears School of Business, where he was a National Honor Scholar, ranking in the top 1% of his class.



