Looking for Expert-Level VA Claim Answers?📱Call Us Now! 737-295-2226
In this updated article, we’ll be exploring the VA disability ratings for Radiculopathy in detail.
VA ratings for Radiculopathy typically range from 0% to 70%, depending upon the severity of your symptoms in terms of frequency (how often), severity (how bad), and duration (how long).
However, VA ratings for Sciatica can range from 10% to 80%, depending upon the severity of symptoms.
The highest possible VA disability rating for Radiculopathy, across all radicular groups, with complete paralysis, is 90%.
Okay, let’s take a minute to explore the law regarding the symptoms and impairment required to warrant a VA disability rating for Radiculopathy.
Many veterans suffer from various back conditions that may or may not be service connected, to include Radiculopathy.
In addition, Radiculopathy is a common secondary VA disability claim, especially Radiculopathy secondary to back conditions or back pain.
Table of Contents
Summary of Key Points
- VA disability ratings for Radiculopathy range from 0% to 90%, depending on the severity, frequency, and duration of symptoms, with Sciatica (a form of Lumbar Radiculopathy) rated under Diagnostic Code 8520 and potentially reaching 80%.
- Radiculopathy can affect four main regions of the spine—cervical, thoracic, lumbar, and sacral—and is rated based on the specific nerve groups involved (e.g., upper/lower extremities) and the level of functional impairment (mild, moderate, severe, or complete paralysis).
- Radiculopathy is commonly rated as a secondary VA disability, especially as a result of service-connected back conditions like spinal stenosis, herniated discs, or spondylolisthesis, and can be claimed alongside primary back conditions under separate ratings.
- Veterans with severe Radiculopathy may also qualify for Special Monthly Compensation (SMC) if they experience loss of use of a hand or foot due to complete paralysis or significant functional loss.
Is Radiculopathy a VA Disability?
Yes, Radiculopathy is a VA disability.
Radiculopathy is most often rated under CFR 38, Part 4, VA Schedule of Ratings, diagnostic codes 8510, 8610, and 8710 for the upper and middle radicular groups.
Paralysis of the Sciatic Nerve, also known as “Sciatica,” is the #7 most common VA disability and is rated under diagnostic codes 8520, 8620, and 8720.
A VA disability rating for Radiculopathy can range from 0% to 90% and depend upon the frequency, severity, and duration of your symptoms, meaning the more severe your symptoms, the higher the VA rating for Radiculopathy.
What is Radiculopathy for VA Disability Rating Purposes?
Your spine is made up of many bones called vertebrae, and your spinal cord runs through a canal in the center of these bones.
Nerve roots split from the cord and travel between the vertebrae into many different areas of your body.
When these nerve roots become pinched or damaged, the resulting symptoms lead to a painful condition called Radiculopathy.
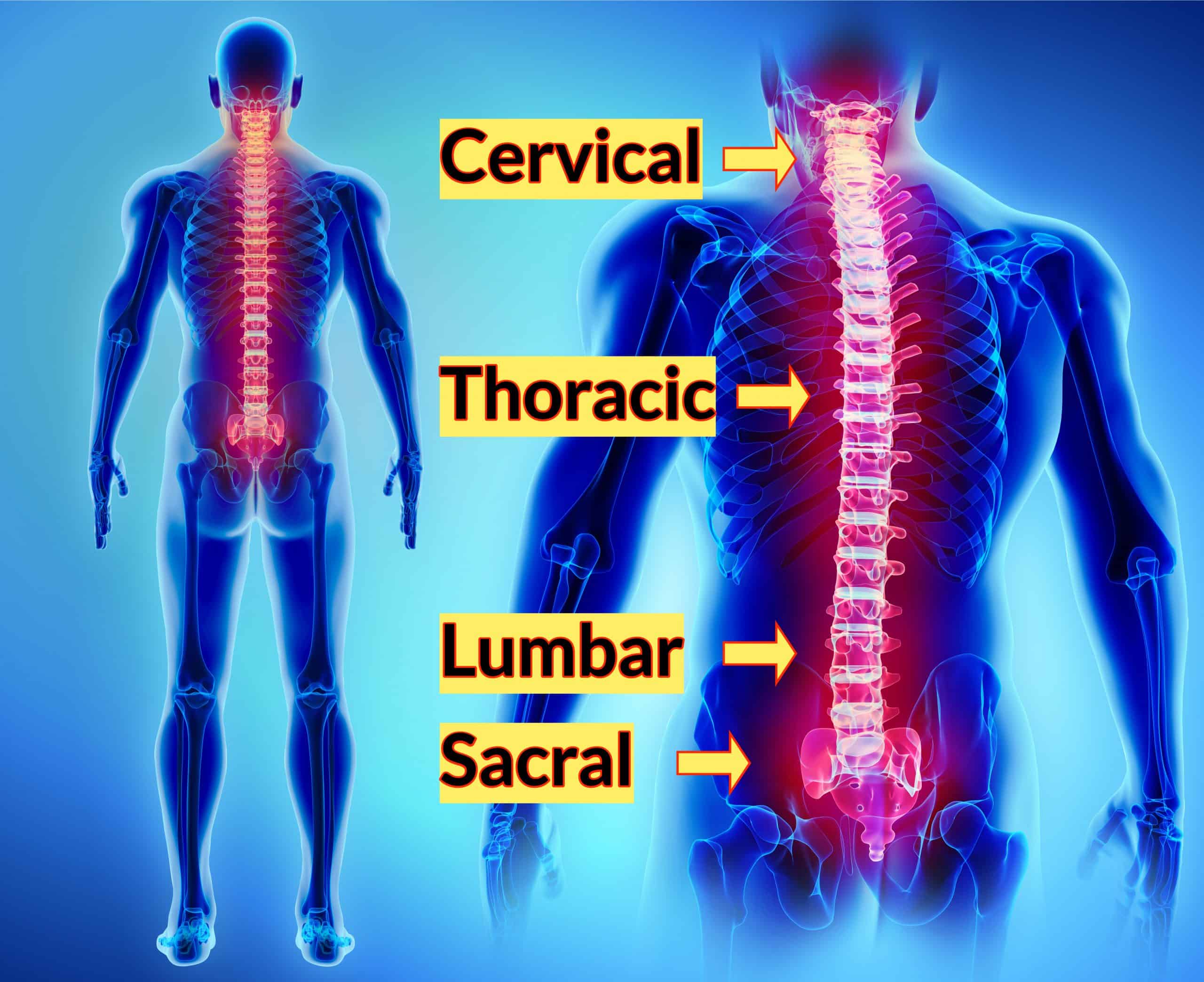
Four Types of Radiculopathy in Veterans
Radiculopathy can have many different signs and symptoms as well as different names depending on where in the spine it occurs.
The spine consists of four (4) primary regions from your neck (cervical spine) down to your buttocks and pelvic area (sacral spine).
The middle and upper back area is your thoracic spine and the lower back area is your lumbar spine.
>> Click HERE to Read About VA Disability Ratings for Spinal Conditions <<
For VA disability purposes, the four regions listed below will be considered when it comes to your final VA rating for Radiculopathy.
But first, let’s explore how the VA looks at Radiculopathy in more detail.
Radiculopathy VA Rating Criteria Explained
The upper and middle radicular group is rated under diagnostic codes 8510, 8610, and 8710.
The sciatic nerve, which is the largest nerve in your body, known as “Sciatica,” is rated under diagnostic codes 8520, 8620, and 8720.
A veterans VA disability rating for Radiculopathy depends upon the frequency, severity, and duration of symptoms, meaning the more severe your symptoms, the higher the VA rating for Radiculopathy.
The Radiculopathy VA rating criteria also depends upon Paralysis, Neuritis, or Neuralgia, as well as the location/region, which are broken down in detail below.
Paralysis
- Complete: This is defined for each nerve a little differently, but basically, it means that the nerve is completely paralyzed, and the body part cannot function at all, like if it had been amputated.
- Incomplete, severe: If the nerve is not completely paralyzed, and there are symptoms, like poor blood circulation and muscle atrophy, that seriously limit the body part’s ability to function, then it is rated as severe. The condition must be very severe to be rated here.
- Incomplete, moderate: If the nerve is not completely paralyzed, and there is tingling, numbness, moderate pain, or other symptoms that significantly interfere with the ability of the body part to fully function, it is rated as moderate.
- Incomplete, mild: If the nerve is not completely paralyzed, and there is only tingling or mild pain in the affected body part, it is rated as mild. There could also be slight or very mild limitations in the movement of the body part, but these limitations would not really affect the overall functioning.
Neuritis
- Severe: If there are all three of the main symptoms (loss of reflexes, muscle atrophy, and loss of sensation), and they seriously limit the body part’s ability to function, then it is rated as severe. The condition must be very severe to be rated here.
- Moderate: If there are one or more of the main symptoms that significantly interfere with the ability of the body part to fully function, it is rated as moderate.
- Mild: If there are one or more of the main symptoms, but they are mild and do not interfere significantly with the ability of the body part to function, it is rated as mild.
Neuralgia
- Moderate: If there is tingling, numbness, moderate to severe pain, or other symptoms that significantly interfere with the ability of the body part to function fully, it is rated as moderate.
- Mild: If there is only tingling or mild pain in the affected body part, it is rated as mild. There could also be slight or very mild limitations in the movement of the body part, but these limitations would not really affect the overall.
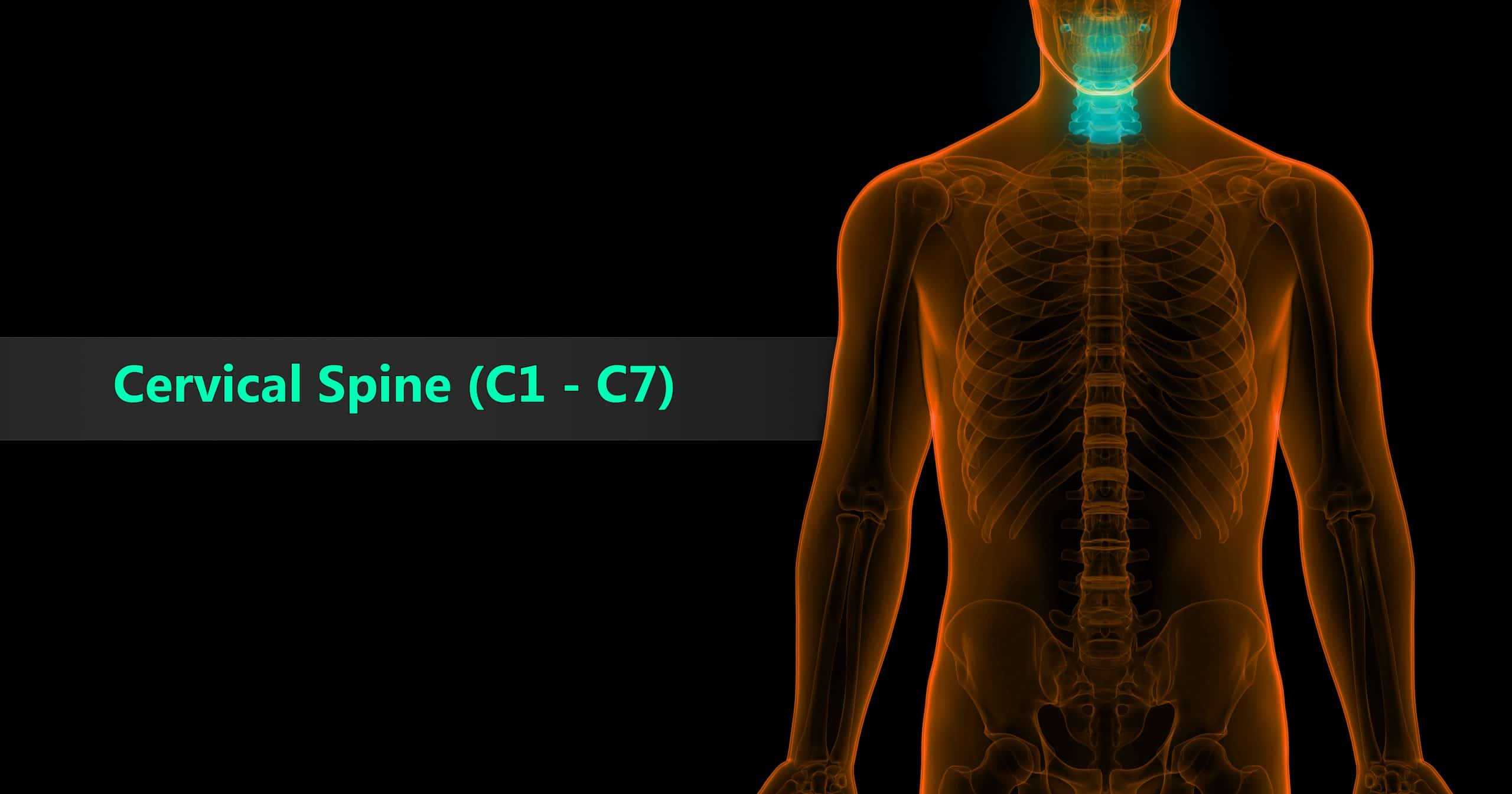
Cervical Spine
The neck region of the spine is known as the Cervical Spine.
This region consists of seven vertebrae, which are abbreviated C1 through C7 (top to bottom).
These vertebrae protect the brain stem and the spinal cord, support the skull, and allow for a wide range of head movement.
The first cervical vertebra (C1) is called the Atlas.
The Atlas is ring-shaped, and it supports the skull. C2 is called the Axis.
It is circular in shape with a blunt peg-like structure (called the Odontoid Process or “dens”) that projects upward into the ring of the Atlas.
Together, the Atlas and Axis enable the head to rotate and turn.
The other cervical vertebrae (C3 through C7) are shaped like boxes with small spinous processes (finger-like projections) that extend from the back of the vertebrae.
Cervical Radiculopathy
Cervical radiculopathy describes a compressed nerve root in the neck (cervical spine).
Because the nerve roots in this area of the spine primarily control sensations in your arms and hands, this is where the symptoms are most likely to occur.
VA Rating for Cervical Radiculopathy
The term “incomplete paralysis,” with this and other peripheral nerve injuries, indicates a degree of lost or impaired function substantially less than the type picture for complete paralysis given with each nerve, whether due to varied level of the nerve lesion or to partial regeneration.
When the involvement is wholly sensory, the rating should be for the mild, or at most, the moderate degree.
The ratings for the peripheral nerves are for unilateral involvement; when bilateral, combine with application of the bilateral factor.
VA Disability Rating for Cervical Radiculopathy
| DC 8510, 8511, 8512, Paralysis of Upper, Middle, and Lower Radicular Groups: | Major | Minor |
| Complete; all shoulder and elbow movements lost or severely affected, hand and wrist movements not affected | 70% | 60% |
| Incomplete: | ||
| – Severe | 50% | 40% |
| – Moderate | 40% | 30% |
| – Mild | 20% | 20% |
| 8610, Neuritis | ||
| 8710, Neuralgia |
Thoracic Spine
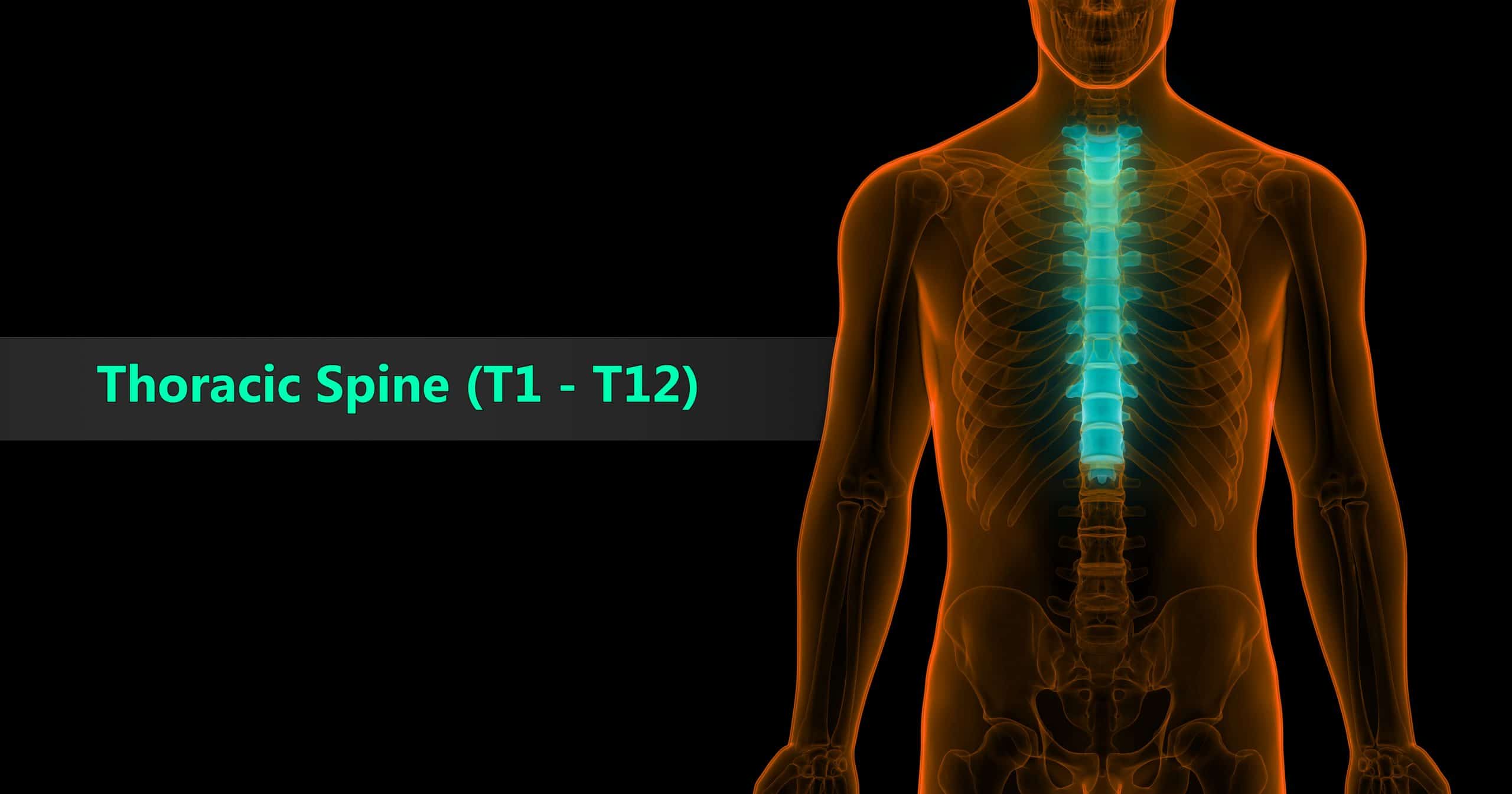
Beneath the last cervical vertebra are the 12 vertebrae of the Thoracic Spine.
These are abbreviated T1 through T12 (top to bottom). T1 is the smallest and T12 is the largest thoracic vertebra.
The thoracic vertebrae are larger than the cervical bones and have longer spinous processes.
In addition to longer spinous processes, rib attachments add to the thoracic spine’s strength.
These structures make the thoracic spine more stable than the cervical or lumbar regions.
In addition, the rib cage and ligament systems limit the thoracic spine’s range of motion and protect many vital organs.
Thoracic Radiculopathy
Thoracic radiculopathy refers to a compressed nerve root in the thoracic area of the spine, which is your middle to upper back.
This is the least common location for radiculopathy.
The symptoms often follow a dermatomal distribution and can cause pain and numbness that wraps around to the front of your body.
VA Disability Rating for the Thoracic Nerve
| DC 8519 Paralysis of: | Major | Minor |
| Complete; inability to raise arm above shoulder level, winged scapula deformity | 30% | 20% |
| Incomplete: | ||
| – Severe | 20% | 20% |
| – Moderate | 10% | 10% |
| – Mild | 0% | 0% |
| Note: Not to be combined with lost motion above shoulder level. | ||
| 8619, Neuritis | ||
| 8719, Neuralgia | ||
| Note: Combined nerve injuries should be rated by reference to the major involvement, or if sufficient in extent, consider radicular group ratings. |
Lumbar Spine
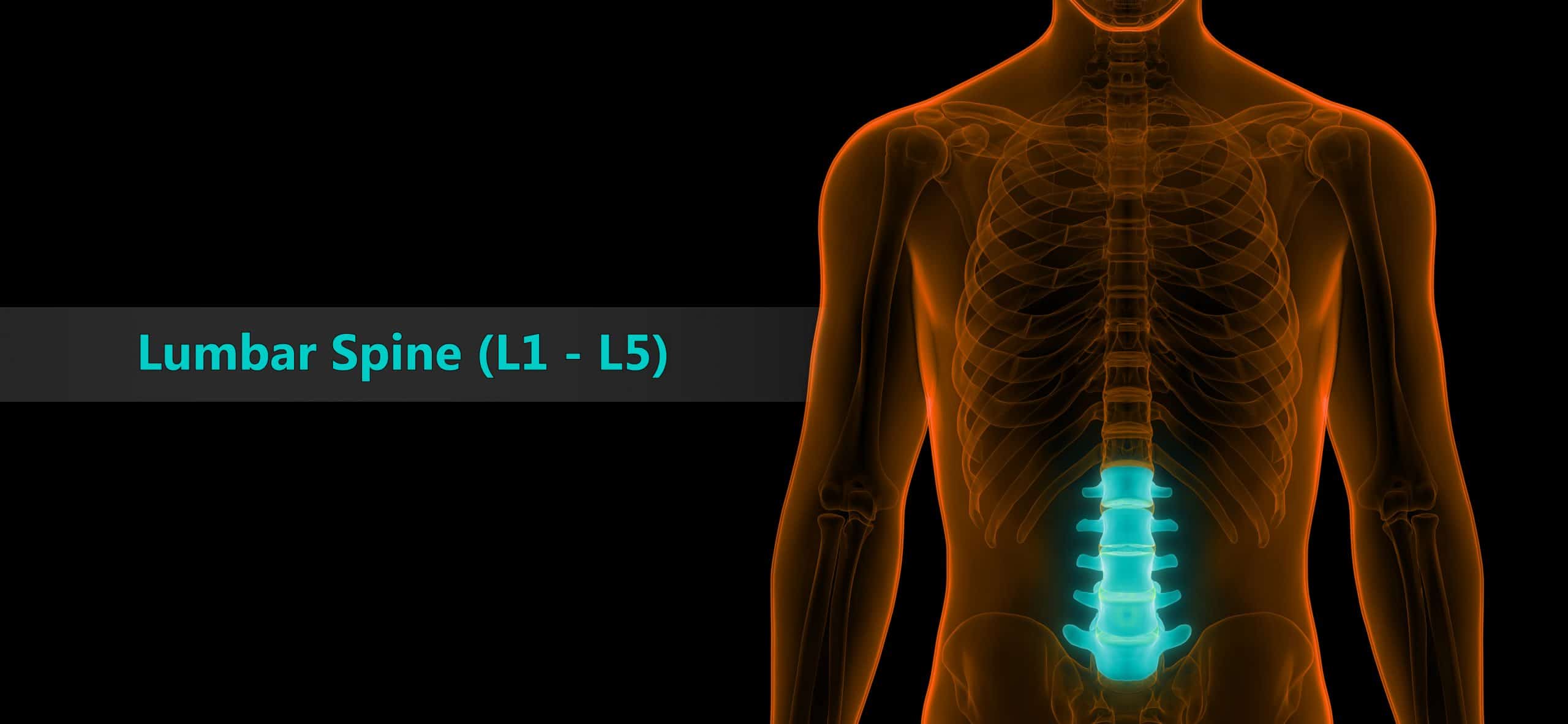
The Lumbar Spine has 5 vertebrae abbreviated L1 through L5 (largest).
The size and shape of each lumbar vertebra is designed to carry most of the body’s weight.
Each structural element of a lumbar vertebra is bigger, wider and broader than similar components in the cervical and thoracic regions.
The lumbar spine has more range of motion than the thoracic spine, but less than the cervical spine.
The lumbar facet joints allow for significant flexion and extension movement but limit rotation.
Lumbar Radiculopathy
When radiculopathy occurs in the lower back, it is known as lumbar radiculopathy, also referred to as sciatica because nerve roots that make up the sciatic nerve are often involved.
The lower back is the area most frequently affected by radiculopathy.
VA Disability Rating for Lumbar Radiculopathy
| DC 8520 Paralysis of: | |
| Complete; the foot dangles and drops, no active movement possible of muscles below the knee, flexion of knee weakened or (very rarely) lost | 80% |
| Incomplete: | |
| – Severe, with marked muscular atrophy | 60% |
| – Moderately severe | 40% |
| – Moderate | 20% |
| – Mild | 10% |
| 8620, Neuritis | |
| 8720, Neuralgia |
Sacral Spine
The Sacrum is located behind the pelvis.
Five bones (abbreviated S1 through S5) fused into a triangular shape, form the sacrum.
The sacrum fits between the two hipbones connecting the spine to the pelvis.
The last lumbar vertebra (L5) articulates (moves) with the sacrum.
Immediately below the sacrum are five additional bones, fused together to form the Coccyx (tailbone).
VA Rating for Radiculopathy Lower Extremity
The VA rating for radiculopathy lower extremity ranges up to 40%, depending on the severity of your symptoms.
In addition, you may receive a separate VA rating for each lower extremity.
VA ratings for Radiculopathy of the left lower and right lower extremities are typically rated under diagnostic code 8620.
The present VA ratings assigned for degenerative joint disease of the lumbar spine, and radiculopathy of the left and right lower extremities when combined (See 38 C.F.R. § 4.23) are rated as 70 percent disabling.
A higher rating than those currently assigned is only provided by rating the service-connected lumbar spine disorders, degenerative joint disease and radiculopathy, separately.
Neuritis of the sciatic nerve is rated under 38 C.F.R. § 4.124a, Diagnostic Code 8621, rather than Diagnostic Code 8626 for rating disability of the anterior crural or femoral nerve.
Incomplete paralysis of the sciatic nerve (sciatica), if severe, with marked muscular atrophy is rated as 60 percent disabling.
Moderately severe incomplete paralysis is rated as 40 percent disabling.
Moderate incomplete paralysis is rated as 20 percent disabling.
VA Rating for Radiculopathy Upper Extremity
VA ratings for upper extremity radiculopathy is rated pursuant to 38 C.F.R. § 4.124a, Diagnostic Code 8710, pertaining to neuralgia or paralysis of the upper radicular group (fifth and sixth cervicals).
Neuralgia of the upper radicular group is rated based on paralysis under Diagnostic Code 8510.
Under that code, mild incomplete paralysis is rated 20 percent disabling for both the major and minor side.
Moderate incomplete paralysis is rated as 40 percent disabling on the major side and 30 percent disabling on the minor side.
A 50 percent rating is warranted for severe incomplete paralysis of the radicular group of the major extremity, and a 40 percent rating is warranted for severe incomplete paralysis affecting the minor extremity.
Symptoms of Radiculopathy in Veterans

When a nerve root is compressed, it becomes inflamed.
This results in numerous unpleasant and painful symptoms in veterans that may include:
- Sharp and radiating pain in the back, arms, legs or shoulders that may worsen with certain activities, even something as simple as coughing or sneezing
- Weakness, fatigue, or loss of reflexes in the arms or legs
- Numbness or tingling of the skin, “pins and needles,” or other abnormal sensations (paresthesia) in the arms or legs
Your specific symptoms will depend on where in the spine the nerve root is pinched.
However, it’s also possible that you don’t experience any symptoms, or you go through periodic flare-ups of symptoms.
Complete paralysis of the upper radicular group, with all shoulder and elbow movements lost or severely affected and hand and wrist movements not affected, warrants a 70 percent rating for the major side and a 60 percent rating for the minor side.
See 38 C.F.R. § 4.124a, Diagnostic Code 8510.
Causes of Radiculopathy in Veterans
Radiculopathy is typically caused by changes in the tissues surrounding the nerve roots.
These tissues include bones of the spinal vertebrae, tendons and intervertebral discs.
When these tissues shift or change in size, they may narrow the spaces where the nerve roots travel inside the spine or exit the spine; these openings are called foramina.
The narrowing of foramina is known as foraminal stenosis, which is very similar to spinal stenosis that affects the spinal cord.
In most cases, foraminal stenosis is caused by gradual degeneration of the spine that happens as you age.
But it can also be a result of a spinal injury.
Herniated Discs
One common cause of foraminal stenosis and radiculopathy is a bulging or herniated
disc.
Spinal discs act as cushions between your vertebrae.
On occasion, these discs slip out of place or become damaged and press on nerves.
This problem is most likely to occur in your lower back, but it can also affect your neck.
Bone Spurs
Another possible cause of radiculopathy that may lead to narrowing of foramina is bone spurs.
Bone spurs are areas of extra bone growth and they can form in the spine due to inflammation from osteoarthritis, trauma, and/or other degenerative conditions.
Other Possible Causes or Radiculopathy in Veterans
Thickening (ossification) of the spinal ligaments may also lead to narrowing of the space around the nerve roots and subsequent nerve compression.
Less common causes of radiculopathy include spinal infections and various cancerous and noncancerous growths in the spine that may press against the nerve roots.
How Veterans Get a Radiculopathy Diagnosis
Your VA doctor or private physician may take several steps to diagnose radiculopathy:
- A physical exam and physical tests may be used to check your muscle strength and reflexes. If you have pain with certain movements, this may help your doctor identify the affected nerve root.
- Imaging tests, such as an X-ray, CT scan or MRI scan, are used to better see the structures in the problem area.
- Nerve conduction studies, along with electromyography, can also be used to help pinpoint whether the problem is neurological or muscular.
Secondary Conditions to Lower Back Pain
Many veterans suffer from various service connected back conditions, which can affect your upper back, middle back, and/or lower back.
For example, the following codes from 38 CFR, Part 4, Schedule for Rating Disabilities apply:
- DC 5237: Lumbosacral or cervical strain—a generic label for back pain
- DC 5238: Spinal stenosis—the spinal column narrows and presses on the spinal cord or nerves
- DC 5239: Spondylolisthesis or segmental instability—when a vertebra slips out of position
- DC 5240: Ankylosing spondylitis—an arthritic disease that causes the spinal joints to freeze in place
- DC 5241: Spinal fusion—the vertebrae are surgically fused together
- DC 5235: Vertebral fracture or dislocation—the bones of the spine break or slip out of alignment due to a traumatic event like a car accident. Any generic spinal bone injury would be coded here.
These six back conditions can often lead to pinched or damaged nerve roots, which can cause significant pain known as Radiculopathy.
Radiculopathy is commonly rated as a secondary VA disability claim for secondary service connection due to one or more service connected back conditions.
Note that a veteran is eligible to be rated for both a back condition, and Radiculopathy secondary to lower back pain.
VA Disability Rating for Radiculopathy: Special Monthly Compensation for Loss of Use of Hand or Foot
Veterans may also qualify for Special Monthly Compensation (SMC) due to loss of use of a hand or foot.
In accordance with §4.63 Loss of Use of a Hand or a Foot, for the purpose of special monthly compensation, will be held to exist when no effective function remains other than that which would be equally well served by an amputation stump at the site of election below elbow or knee with use of a suitable prosthetic appliance.
The determination will be made on the basis of the actual remaining function of the hand or foot, whether the acts of grasping, manipulation, etc., in the case of the hand, or of balance and propulsion, etc., in the case of the foot, could be accomplished equally well by an amputation stump with prosthesis:
- (a) Extremely unfavorable complete ankylosis of the knee, or complete ankylosis of 2 major joints of an extremity or shortening of the lower extremity of 31⁄2 inches (8.9 cms.) or more, will be taken as loss of use of the hand or foot involved.
- (b) Complete paralysis of the external popliteal nerve (common peroneal) and consequent, footdrop, accompanied by characteristic organic changes including trophic and circulatory disturbances and other concomitants confirmatory of complete paralysis of this nerve, will be taken as loss of use of the foot.
Fellow Veterans Please Remember This Fact: YOU SERVED. YOU DESERVE.
Don’t ever stop fighting for the benefits you earned through your service to our country!
At VA Claims Insider, we’re here to help you maximize your benefits and secure the compensation you rightfully deserve.
We’ve helped 25,000+ veterans increase their VA rating—YOU could be next!
Let’s get you the VA disability benefits you deserve.
If you need expert help navigating the VA claims process, our team of VA claim coaches is ready to educate and empower you to victory!
✅ If you’re sick and tired of waiting and want expert guidance to get the VA rating and compensation you deserve faster, CALL US RIGHT NOW at 737-295-2226 for a no-obligation VA claim consultation!
Want Expert-Level Help With Your VA Claim? WE GOT YOUR SIX!
How does VA Claims Insider help veterans?
We make the confusing and frustrating VA claim process EASY through our 8-step proprietary system and one-on-one coaching; we’re the VA Claim EXPERTS you can trust, and YOU are never alone in this fight against the VA!
You’ll also receive VA disability expert Brian Reese’s SEM Method Blueprint—a proven formula that has helped over 25,000 veterans win their VA disability claims faster:
Strategy + Education + Medical Evidence = VA Rating and Compensation You Deserve FASTER!
Start today and unlock an exceptional level of service you deserve for serving our country:
➡️ You’ll hear from a VA Claim Expert over email within 15 minutes of signing up today.
➡️ You’ll hear from your Veteran Coach team within 24 hours of all inquiries during normal business days/hours.
➡️ Our terms are simple: IF WE DON’T WIN, YOU DON’T PAY. You have nothing to lose and everything to gain!
Click the red button below to start the process of winning your VA claim right now:
Fellow Veterans: Are You Ready to WIN, SERVICE-CONNECT, and INCREASE Your VA Disability Rating FASTER? We Can Help!
- VA Claims Insider is the #1 most trusted name in VA disability claims.
- Work directly with a VA claims coach who can help lead you to VA claim victory.
- 25,000+ disabled veterans served in our membership programs since 2016.
- 30% average rating increase for veterans who complete our #1 rated Elite program.
- 4.7/5.0 average rating out of 5,500+ total reviews; over 4,500 5-star reviews.
About The Author

Brian Reese
Brian Reese is a world-renowned VA disability benefits expert and the #1 bestselling author of VA Claim Secrets and You Deserve It. Motivated by his own frustration with the VA claim process, Brian founded VA Claims Insider to help disabled veterans secure their VA disability compensation faster, regardless of their past struggles with the VA. Since 2013, he has positively impacted the lives of over 10 million military, veterans, and their families.
A former active-duty Air Force officer, Brian has extensive experience leading diverse teams in challenging international environments, including a combat tour in Afghanistan in 2011 supporting Operation ENDURING FREEDOM.
Brian is a Distinguished Graduate of Management from the United States Air Force Academy and earned his MBA from Oklahoma State University’s Spears School of Business, where he was a National Honor Scholar, ranking in the top 1% of his class.