Looking for Expert-Level VA Claim Answers?📱Call Us Now! 737-295-2226
Today, we’re going in-depth to examine the VA rating for migraines.
Migraine headaches are rated as follows: 0%, 10%, 30%, or 50%.
The highest scheduler VA disability rating for migraines is 50%.
Brian Reese here! I’m an Air Force service-disabled veteran, VA disability expert, and founder of VA Claims Insider—the most trusted name in VA disability claims.
This is NOT your average “VA disability rating for migraines” prediction post.
Yes, I cover the most important migraine headaches VA rating trends.
But you’re also going to get real BVA (Board of Veterans Appeals) case law and cutting-edge medical research studies that support a relationship between migraine headaches and other service-connected disabilities.
So, regardless of your current VA disability rating for migraines, this new guide will help you win, service-connect, and get a higher VA rating for headaches, regardless of previous denials.
Table of Contents
Are Headaches a VA Disability?
Yes, headaches are a VA disability.
They fall under CFR 38, the schedule for rating disabilities, diagnostic code 8100 for migraines.
In fact, according to the Veterans Benefits Administration (VBA) and the Top 10 Most Common VA Disability Claims, migraines are the #9 most commonly claimed VA disability.
Types of Headaches for VA Rating Purposes
While the law only specifically lists migraines as a ratable VA disability condition, ANY type of headache condition can receive a VA rating if you have symptoms that affect your work, life, and functioning due to your military service or another service-connected disability.
The International Headache Society and the Mayo Clinic have identified more than 150 different types of headaches, which are divided into three categories: Primary, Secondary, and Other.

For example, tension headaches are the most common type of headache among adults and the most common type of headache in veterans as well.
They cause mild to moderate pain and come and go over time.
They usually have no other symptoms.
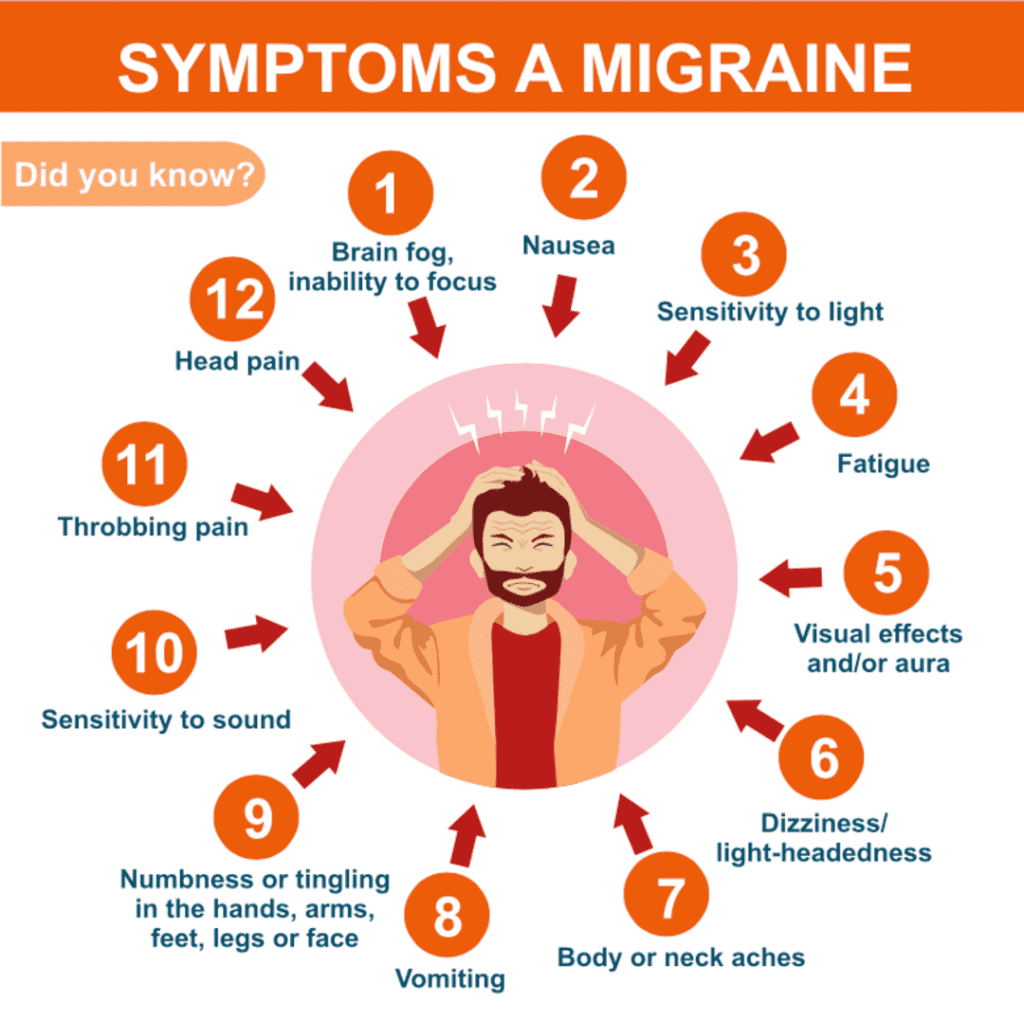
Migraine headaches are often described as pounding, throbbing pain.
They can last from 4 hours to 3 days and usually happen one to four times a month.
Along with the pain, people may have other symptoms, such as sensitivity to light, noise, or smells; nausea or vomiting; loss of appetite; and upset stomach or belly pain.
Post-traumatic headaches, for example, are quite common among veterans, specifically if you suffered from any type of head injury or trauma during military service.
Furthermore, post-traumatic headaches, particularly migraine headaches, are commonly found in veterans who deployed in support of combat operations in Iraq and Afghanistan.
According to medical research, if you get a new headache within seven to 10 days of your head injury or after you’re conscious again from the trauma, you may have a condition known as a post-traumatic headache.
The Term “Prostrating” Will Make or Break Your VA Claim for Migraines
What is a “Prostrating” Migraine Headache?
Perhaps the single most important term that can literally make or break your VA rating for migraines is the word “prostrating.”
The reason it’s so important is because the 30% and 50% VA ratings for migraines contain the word “prostrating” in reference to both the frequency and severity of your condition.
What’s interesting is that neither VA regulations nor the courts have attempted to define the term “prostrating.”
By way of reference, according to Merriam-Webster’s Collegiate Dictionary 999 (11th Ed. 2007), “prostration” is defined as “complete physical or mental exhaustion.”
A very similar definition is found in Dorland’s ILLUSTRATED MEDICAL DICTIONARY 1554 (31st Ed. 2007), in which “prostration” is defined as “extreme exhaustion or powerlessness.”
The best definition we could find for “prostrating” comes from Dictionary.com:
“To lay oneself flat on the ground face downward, especially in reverence or submission.”
Prostrating is further defined as weakness, fatigue, distress, exhaustion, illness, or functional loss, for example:
“To reduce (someone) to extreme physical weakness.”

Statement in Support of a Claim for Migraines
In the absence of service treatment records or current symptoms of migraine headaches, a Statement in Support of Claim can be extremely helpful documentation to strengthen your claim.
A well-done Statement in Support of a Claim can help to complete what is known as a fully-developed claim, which is a well-supported, complete presentation of your case that has a higher likelihood of winning and tends to be approved faster. (We specialize in helping veterans build and win claims this way!)
For a Statement in Support of Claim (personal statement) you’ll need to use form VA 21-4138. At VA Claims Insider we highly recommend taking advantage of VA Form 21-4138 to provide key supporting evidence for most claims, and definitely for migraine claims.
(While we used to recommend “buddy letters” from first-hand witnesses for these and other claims, over time, we’ve seen buddy letters “muddy the waters” and hurt more than help a claim. Conflicting information from lay witnesses can actually slow down your claim and even lead to denial.
Therefore, we now recommend that you skip the “buddy letter” example or lay witness statements and stick to your own well-crafted personal statement. That way, you control the narrative, the wording and the details and can ensure consistency.)
You can learn more about writing a great personal statement from this video: “How to Write a WINNING VA Statement in Support of Claim! (4-Step Process)
There are keyword combinations you should be sure to use in your personal statement, as well as when you speak to your VA doctor and at your VA C&P Exam.
Assuming you really do have severe symptoms, your wording (in writing in your personal statement, verbally to your doctor, and at a C&P exam) might sound like this):
“My headaches are so severe that when I get an attack—which happens three to four times per week—I end up having to lie down in a dark room for hours until they stop. This has affected my work, life, and social functioning. In fact, I’m now unemployed because I couldn’t perform the functions of my job due to the severity and frequency of my headaches.”“My migraines cause extreme radiating pain from my neck all the way up through both sides of my head. When I’m having a migraine, I end up taking sick leave from work because I must lie down by myself in a quiet room.”
VA Rating for Migraines Criteria
CFR 38, Part 4, the Schedule for Rating Disabilities, lists migraines under code 8100.
The migraines VA rating scale consists of four rating possibilities: 0%, 10%, 30%, and 50%.
The symptoms become markedly more severe between the 30% and 50% rating levels, as evidenced by the rating criteria below:
| 8100, migraine headaches: | Rating |
| Migraines with very frequent completely prostrating and prolonged attacks productive of severe economic indaptability | 50% |
| Migraines with characteristic prostrating attacks occurring on an average once a month over last several months | 30% |
| Migraines with characteristic prostrating attacks averaging one in 2 months over last several months | 10% |
| Migraines with less frequent attacks | 0% |
How to Get 50% VA Disability for Migraines
There is a significant difference between the 30% rating for migraines and the 50% rating for migraines.
For example, look at this actual denial letter from a VA Rater for a veteran who was already ready at 30% for migraines but was seeking an increase to 50% for migraines:
“Although the medical evidence shows that the frequency of the headaches has increased, there is no objective medical evidence showing that these headaches are at all prostrating in nature which would affect economic inadaptability. However, based on the totality of the evidence which includes the veteran’s subjective statements, and resolving all reasonable doubt in his favor, we feel that the 30% rating threshold has been met justifying an increase at this time. A higher evaluation is not warranted unless the objective medical evidence shows very frequent, completely prostrating, and prolonged attacks productive of severe economic inadaptability.”
Medical Evidence Requirements for Migraines
The denial states the medical evidence did NOT show prostrating headaches or economic loss.
If you think you deserve a higher VA rating for migraines, you need to have medical evidence that discusses the severity of your headaches, whether they are prostrating in nature, and if these headaches affect your work.

The best way to do this is to get a Disability Benefits Questionnaire (DBQ) for migraines completed by a qualified medical professional.
If you’re already service-connected for migraines at 0% or higher, this is a simple increase based on new and relevant medical evidence (the DBQ report).
Sometimes, a VA Rater will accept a migraines DBQ on its own and grant the rating increase without a C&P exam.
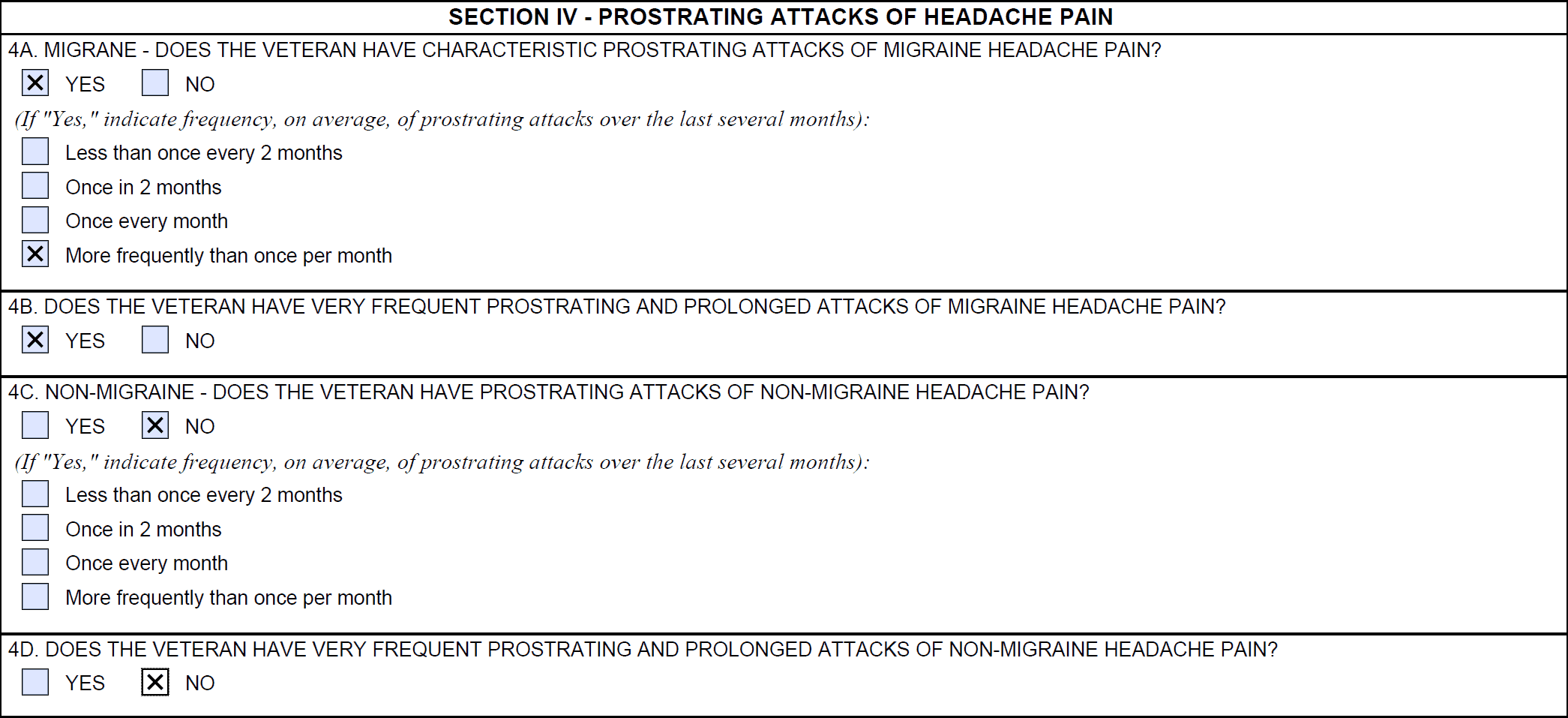
The most important section of the DBQ for migraines is Section IV – Prostrating Attacks of headache pain.
If your migraines are so severe that you often need to lie down in a dark room for hours, which indicates “Prostrating” attacks, make sure to tell your doctor about it and ensure the DBQ is completed correctly.
Another tip for VA claims for migraines is you need to be documenting the frequency and severity of your migraines over the past several months, so you have additional evidence.
You can use apps on your smartphone, such as the Migraine Buddy app, from which you can then download the daily and monthly reports to use in support of your VA claim for headaches.
30% VA Rating for Migraines
At the 30% VA rating for migraines, the law lists headaches “with characteristic prostrating attacks occurring on an average once a month over the last several months.”
Note the keyword “prostrating,” meaning you’ve had to lie down.
You can also see that the 30% rating has prostrating attacks that occur roughly one time per month over the past several months.
There is no mention of any functional or economic loss.
50% VA Rating for Migraines
At the 50% VA rating for migraines, the law describes headaches “with very frequent completely prostrating and prolonged attacks productive of severe economic inadaptability.”
Note the keywords “very frequent completely prostrating,” meaning you’ve had to lie down more often, and the migraines could last for extended periods of time.
You can also see that the 50% rating introduces “severe economic inadaptability.”
Regarding the term “productive of economic inadaptability,” the case law precedent indicates that “productive of” can also mean “producing” or “capable of producing.”
Further, the term “inadaptability” has NEVER been defined by the courts, nor can a definition be found anywhere in 38 CFR.
The term “severe economic inadaptability” refers to a veteran’s inability to work, but NOTHING in the Migraines Diagnostic Code 8100 requires that the veteran be completely unable to work in order to qualify for a 50% rating.
Therefore, a veteran can qualify for a 50 percent VA rating for migraines and still be working or able to work.
For example, maybe you’ve been fired from a job because you missed work so often due to the severity of your migraines.
Perhaps you have severe migraines on a weekly basis, and you’ve used all your sick leave at work and it’s now affecting your ability to produce and earn a living, but you’re still working.
Expert Tips to Service-Connect Your Migraines
Many veterans unsuccessfully attempt to service-connect migraines as a primary disability (direct service connection).
The problem is you probably weren’t diagnosed with migraines while on active duty, and it’s now years later, meaning it will be difficult to prove direct service connection.
But is there maybe a better way?
There is!
And it’s an expert level tip from Brian Reese and the VA Claims Insider.
Migraines and Secondary Service Connection
Migraines and many other types of headaches can be medically linked to numerous other service-connected disabilities.
Thus, it’s possible for veterans to seek service connection on a secondary basis, which requires a showing of causation.
A showing of causation requires that the secondary disability be shown to be “proximately caused by” or “proximately aggravated by” another service-connected disability.
Accordingly, service connection may be granted on a secondary basis for a disability that is proximately due to, the result of, or aggravated by a service-connected disability. See 38 C.F.R. § 3.310(a) and (b) (2014). Also see Allen v. Brown, 7 Vet. App. 439, 448 (1995).
By law, there are three essential elements that must be satisfied to service-connect migraines as a secondary condition
- A medical diagnosis of migraines or any other type of headache condition
- Evidence of a service-connected primary disability (such as TBI, tinnitus, PTSD, depression, anxiety, sinusitis, rhinitis, cervical strain), AND
- Medical nexus evidence establishing a connection (nexus) between the current disability (migraines) as proximately due to, the result of, or aggravated by another service-connected disability rated at 0% or higher.
The first part can be satisfied with any existing medical evidence in service treatment records, VA medical records, or any private medical records.
The second part can be satisfied with a veteran’s existing service-connected disability rated at 0 percent or higher.
The third part can be satisfied with a medical nexus letter from a qualified medical professional.
You DESERVE a HIGHER VA rating.
Take advantage of a VA Claim Discovery Call with an experienced Team Member. Learn what you’ve been missing so you can FINALLY get the disability rating and compensation you’ve earned for your service.
List of VA Secondary Conditions Due to Migraines
Headaches are often granted secondary service connection because the disability (migraine headache) is shown to be proximately due to, the result of, or aggravated by another service-connected disability.
The frequency and severity of headache conditions typically increase with the severity of other service-connected disabilities.
For example, veterans with more severe PTSD symptoms are likely to have more severe Migraine Headache symptoms, suggesting a correlation between the two.
There are many possible links for veterans to establish secondary service connection for Migraines, including, but not limited to:
Migraines Secondary to Tinnitus
Research suggests that there is a connection between headaches and tinnitus. The symptoms go hand in hand with many types of headaches, including migraines and hypertension. Recent results show 27% of tinnitus sufferers also suffer from headaches. Thus, there is a clear medical etiology to suggest that migraines and many types of headaches can be proximately due to or aggravated by tinnitus, aka ringing in the ear syndrome.
Migraines Secondary to TBI
There are several research studies linking Traumatic Brain Injury (TBI) to migraines as well as post-traumatic headaches. A 2012 study of soldiers returning from combat found that chronic daily headaches were “considerably more common” than might be expected. For example, one study concluded that 29% of soldiers who deployed and suffered from mild TBI also had Migraines.
Migraines Secondary to TMJ
Research has shown that people who grind or clench their teeth are more likely to have migraines than those who don’t. Thus, there is a medical link between migraines and TMJ or TMD.
A similar body of research suggests that the trigeminal nerve plays an important role in the start of a migraine attack. The trigeminal nerve sends signals to the blood vessels and lining of the brain, leading to cortical spreading depression (CSD—a wave of activity that propagates across the brain surface) and a release of chemicals that result in the pain and throbbing of a migraine headache.
Further, neck and jaw problems are a common cause of migraine headaches. Here’s a 2011 BVA case that granted Migraine Headaches secondary to TMJ.
Migraines Secondary to PTSD
Research suggests a connection between migraines and Post-Traumatic Stress Disorder, especially in military veterans. Patients with migraine or tension headaches report high rates of exposure to traumatic events. In addition, about 17% have symptoms consistent with a PTSD diagnosis.
PTSD can also significantly interfere with many aspects of a veteran’s life, including work, life, and social functioning. This fact likely causes more stress, which increases the likelihood of headaches.
Here’s an example of a BVA case decision from 2015 that granted secondary service connection for Migraine Headaches secondary to PTSD. Interestingly, the VA C&P examiner concluded it was less likely than not that the veteran’s headaches are proximately due to or aggravated by his PTSD.
However, the veteran had two positive medical nexus opinions from private providers, affirming that it was “more likely than not” that the headaches were a result of PTSD.
Thus, in view of the totality of the evidence, the Board finds that the evidence is at least in “equipoise” as to whether the Veteran’s current headaches are proximately due to his PTSD. Accordingly, service connection for headaches secondary to service-connected PTSD is granted.
Migraines Secondary to Depression
There is a growing body of evidence that suggests a link between migraines, headaches, and depression, although it’s not entirely clear as of 2022. The most likely link to help a veteran connect migraines secondary to depression is through an “interim link.” This means migraines that are proximately due to or aggravated by service-connected depression—specifically, the side effects of antidepressant medications.
Many SSRIs (selective serotonin reuptake inhibitors—a common type of antidepressant) have serious side effects, including nausea, vomiting or diarrhea, migraines and other types of headaches, drowsiness, dry mouth, insomnia, nervousness, agitation or restlessness, dizziness, sexual problems (such as reduced sexual desire, difficulty reaching orgasm, or inability to maintain an erection/erectile dysfunction), and impact on appetite, weight loss or weight gain.
Migraines Secondary to Anxiety
Researchers have suggested that a link exists between anxiety disorders and migraines. Migraines and chronic daily headaches are common in people who suffer from anxiety disorders, especially in veterans who are already service-connected for a mental health condition, such as PTSD, depression, or anxiety.
Many studies have found that people with Generalized Anxiety Disorder (GAD) and panic disorder experience migraines or other types of headaches at a much higher rate than those without a mental health condition.
Again, in our experience, the best way to service-connect migraines secondary to anxiety is through the interim medical side effects method listed above.
Migraines Secondary to Somatic Symptom Disorder
There is a strong medical link between Migraines and Somatic Symptom Disorder. One study concluded, “Associated somatic symptoms are more common in patients with migraines, with more frequent severe headaches, and with associated anxiety or depression.” Headache disorders may be characterized as showing increasing somatic prevalence as headaches become more frequent.
Migraines Secondary to Sinusitis
A growing body of research links migraines to sinus conditions such as Sinusitis. In the recent American Migraine Study II, 40% to 70% of respondents with migraine headaches had comorbid allergies (meaning they occurred together). Research studies show how commonly sinus symptoms are linked with migraine. Specifically, in one such study, 45% of patients with migraines had symptoms of sinusitis, such as head and nose pressure and pain, nasal congestion, and runny nose.
Migraines Secondary to Rhinitis
Research studies have concluded that people with Rhinitis are more than ten times more likely to have migraines. Thus, there is a very strong link associating migraines with rhinitis, which opens the path for secondary service connection. Some studies have shown that up to 90% of sinus headaches are actually migraines.
Migraines Secondary Cervical Strain (Neck Condition)
The most common symptoms of cervical disorders such as cervical strain are suboccipital cervicogenic headache and ongoing or motion-induced neck pain. Thus, there is a medical nexus (link) connecting migraines to cervical strain, allowing for secondary service connection. Here’s a recent BVA case from 2015 that granted occipital headaches secondary to cervical spine degenerative disc disease (DDD).

Migraines Secondary to Sleep Apnea
In patients who suffer from moderate to severe sleep apnea, headaches have been medically linked to the condition. This is especially true when oxygen levels drop due to the intermittent breathing associated with obstructive sleep apnea (OSA).
Sleep apnea causes air to be trapped in the lungs, and this de-oxygenated air is the waste product of carbon dioxide. This lack of oxygen in the bloodstream, along with carbon dioxide, negatively affects the brain and leads to headaches, which can include migraines.
Migraines Secondary to Radiculopathy
Medical research shows a strong correlation between migraines and radiculopathy, especially when the upper nerve roots are involved. Patients have reported this pinched nerve in the neck leads to more serious headaches, such as migraines. It should be noted, however, that headaches caused by lower nerves in the neck are more common than upper nerve-related headaches.
Migraines Secondary to Asthma
There is a strong correlation between migraines and asthma. One research study reported that people with migraines are 2 to 3.5 times more likely to have or develop asthma.
Migraines Secondary to Medication Side Effects
Literally thousands of over-the-counter medications and prescription medications, especially selective serotonin reuptake inhibitors (SSRIs), can cause or worsen migraines and headaches in general. If you’re a veteran who takes medications to help manage the daily chronic pain or mental health conditions, and you now have headaches, you can likely get service-connected for migraines secondary to medication side effects.
How to File a VA Claim for Migraines
About the Author

Brian Reese
Brian Reese is a world-renowned VA disability benefits expert and the #1 bestselling author of VA Claim Secrets and You Deserve It. Motivated by his own frustration with the VA claim process, Brian founded VA Claims Insider to help disabled veterans secure their VA disability compensation faster, regardless of their past struggles with the VA. Since 2013, he has positively impacted the lives of over 10 million military, veterans, and their families.
A former active-duty Air Force officer, Brian has extensive experience leading diverse teams in challenging international environments, including a combat tour in Afghanistan in 2011 supporting Operation ENDURING FREEDOM.
Brian is a Distinguished Graduate of Management from the United States Air Force Academy and earned his MBA from Oklahoma State University’s Spears School of Business, where he was a National Honor Scholar, ranking in the top 1% of his class.