Looking for Expert-Level VA Claim Answers?📱Call Us Now! 737-295-2226
Post-Traumatic Stress Disorder (PTSD) is currently the #6 most common VA disability claim and the #1 most prevalent service-connected mental health condition among veterans.
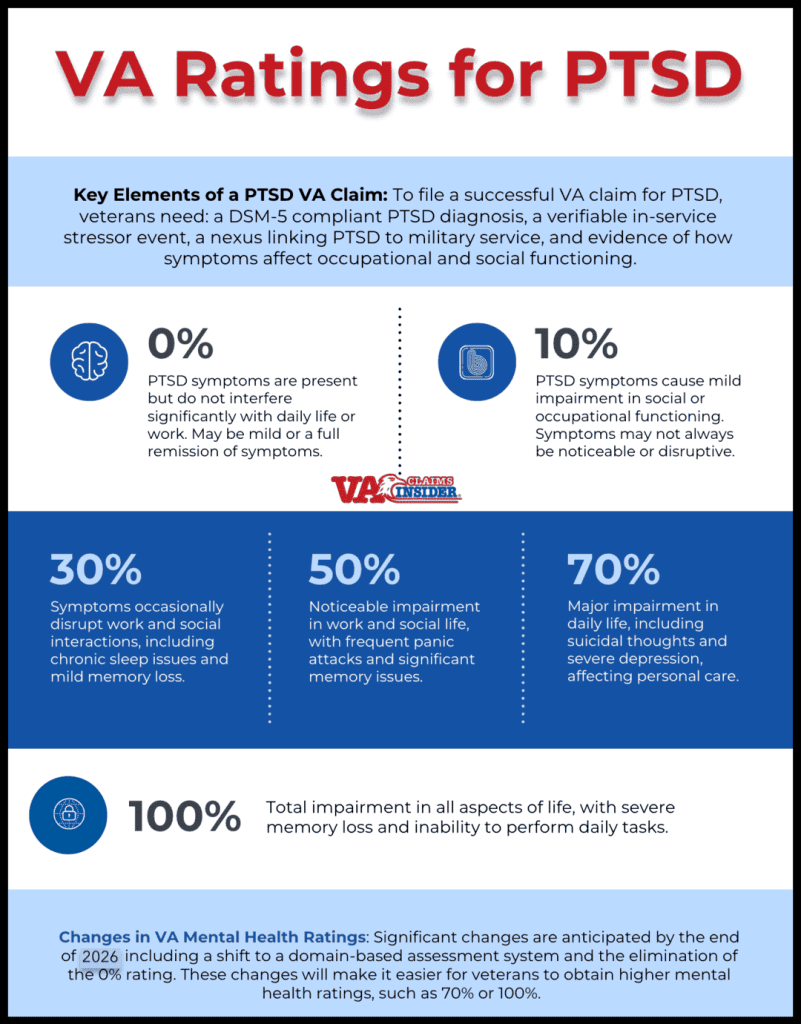
If you’re navigating the VA claims process for PTSD, it’s crucial to understand the key components of a successful claim: (1) a diagnosis of PTSD that conforms to DSM-5 standards, (2) a verifiable in-service stressor event, (3) a ‘nexus’ connecting your PTSD to your military service, and (4) evidence of the severity of symptoms and how these symptoms impact your occupational and social functioning.
In this article, we’ll explore the current VA rating criteria for PTSD, explain how the VA determines your PTSD rating, examine proposed changes to VA mental health conditions, including PTSD, and share tips and strategies for your PTSD C&P exam.
Summary of Key Points
- Prevalence of PTSD in Veterans: PTSD is the most prevalent service-connected mental health condition among veterans, and the #6 most common VA disability claim overall.
- Key Elements of a PTSD VA Claim: To file a successful VA claim for PTSD, veterans need: a DSM-5 compliant PTSD diagnosis, a verifiable in-service stressor event, a nexus linking PTSD to military service, and evidence of how symptoms affect occupational and social functioning.
- VA PTSD Ratings: The VA rates PTSD from 0% to 100% with breaks at 10%, 30%, 50%, and 70%, based on the severity of symptoms and their impact on work and social life. Ratings are outlined under 38 CFR § 4.130 (the mental health rating schedule) in the VA’s Schedule for Rating Disabilities under Diagnostic Code 9411.
- Upcoming Changes in VA Mental Health Ratings: Significant changes are anticipated by the end of 2026, including a shift to a domain-based assessment system and the elimination of the 0% rating. These changes will make it easier for veterans to obtain higher mental health ratings, such as 70% or 100%.
Table of Contents
VA Rating for PTSD
A VA rating for PTSD ranges from 0% to 100% with breaks at 10%, 30%, 50%, and 70%.
The VA rates PTSD based on the severity of symptoms and the level of impairment they cause in both occupational (work) and social (life) functioning.
The PTSD rating chart is outlined in the VA’s Schedule for Rating Disabilities (VASRD), Diagnostic Code (DC) 9411.
0% PTSD Rating
PTSD symptoms are present but do not interfere significantly with social or occupational functioning. There may be mild symptoms or a full remission of symptoms.
A veteran may have occasional nightmares or mild anxiety but is otherwise able to function normally in daily life and work.
10% PTSD Rating
PTSD symptoms cause mild impairment in social or occupational functioning. Symptoms may not always be noticeable or disruptive.
The veteran experiences occasional sleep disturbances, mild anxiety, or mild hypervigilance but can generally maintain relationships and employment.
30% PTSD Rating
PTSD symptoms cause occasional decreases in work efficiency and intermittent periods of inability to perform occupational tasks, though generally functioning satisfactorily with routine behavior, self-care, and conversation.
The veteran has occasional panic attacks, chronic sleep impairment, or mild memory loss.
They may struggle with work-related stress or find social interactions somewhat challenging but are generally able to cope.
50% PTSD Rating
PTSD symptoms cause reduced reliability and productivity due to disturbances such as flattened affect, frequent panic attacks, impaired judgment, difficulty in understanding complex commands, impaired short- and long-term memory, disturbances of motivation and mood, and difficulty in establishing and maintaining effective work and social relationships.
The veteran has frequent panic attacks, experiences mood swings, and has difficulty maintaining work performance or social relationships.
They may struggle with tasks that require concentration and tend to avoid social interactions.
70% PTSD Rating
PTSD symptoms cause deficiencies in most areas such as work, school, family relations, judgment, thinking, or mood, due to symptoms like suicidal ideation, obsessional rituals interfering with routine activities, speech intermittently illogical, obscure, or irrelevant, near-continuous panic or depression affecting the ability to function independently, appropriately and effectively, impaired impulse control, neglect of personal appearance and hygiene, difficulty in adapting to stressful circumstances, inability to establish and maintain effective relationships.
The veteran experiences near-continuous panic or depression and has significant difficulty in social and work settings, and may exhibit neglect of personal hygiene.
They might also have severe issues with anger management or find it impossible to maintain stable relationships.
The 70% rating is the most common rating among veterans with service-connected PTSD.
100% PTSD Rating
PTSD symptoms result in total occupational and social impairment, due to symptoms such as gross impairment in thought processes or communication, persistent delusions or hallucinations, grossly inappropriate behavior, persistent danger of hurting self or others, intermittent inability to perform activities of daily living, disorientation to time or place, memory loss for names of close relatives, own occupation, or own name.
The veteran is unable to work or maintain any social relationships.
They may have severe memory loss, experience hallucinations, or exhibit dangerous behavior.
They might also be disoriented or unable to perform basic daily activities.
2026 VA PTSD Rating Pay Chart
Here are the 2026 VA pay rates for PTSD by disability rating with no dependents:
- 10% Rating: $180.42 per month
- 20% Rating: $356.66 per month
- 30% Rating: $552.47 per month
- 40% Rating: $795.84 per month
- 50% Rating: $1,132.90 per month
- 60% Rating: $1,435.02 per month
- 70% Rating: $1,808.45 per month
- 80% Rating: $2,362.30 per month
- 90% Rating: $2,297.96 per month
- 100% Rating: $3,938.58 per month
If you have dependents, your monthly pay rate will be higher if you have a rating of 30% or more, as there is no additional compensation for dependents with a 10% or 20% VA rating.
These pay rates reflect the 2026 cost-of-living adjustment (COLA) increase of 2.8%.
How the VA Determines Your PTSD VA Rating
Your PTSD VA rating is based on a thorough evaluation of your symptoms and their impact on your daily life, particularly in terms of occupational and social functioning.
Here’s an overview of the process:
1. Diagnosis and Medical Evidence
To establish a valid PTSD VA claim, the veteran must have a current diagnosis of PTSD that meets the criteria set forth in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5).
This diagnosis must come from a qualified mental health professional, such as a psychiatrist or psychologist.
The C&P examiner will make or confirm your PTSD diagnosis on exam day.
2. In-Service Stressor Event
The veteran must demonstrate a connection between their PTSD and an in-service stressor event.
This can be verified through military records, personal statements, or corroborative evidence from other sources.
The VA has a new VA Form 21-0781 to help validate your PTSD stressor event.
3. Nexus (Link or Connection)
There must be a clear “nexus,” or link, between the in-service stressor and your PTSD.
This is typically established through medical evidence, including statements from healthcare providers that explicitly connect the PTSD to the veteran’s service.
If you’ve been out of the military for more than 12 months, it’s highly recommended to get an independent psychological evaluation before filing your PTSD claim.
4. Evaluation of Symptoms
Finally, the VA Rater will assign a PTSD rating based on the severity of symptoms in terms of frequency, severity, and duration, along with how those symptoms affect occupational and social impairment.
The VA Disability Benefits Questionnaire (DBQ) for PTSD includes a comprehensive list of 31 mental health symptoms used to evaluate the severity of your PTSD:
- Depressed mood
- Anxiety
- Suspiciousness
- Panic attacks that occur weekly or less often
- Panic attacks more than once a week
- Near-continuous panic or depression affecting the ability to function independently, appropriately, and effectively
- Chronic sleep impairment
- Mild memory loss, such as forgetting names, directions, or recent events
- Impairment of short and long-term memory, for example, retention of only highly learned material, while forgetting to complete tasks
- Memory loss for names of close relatives, own occupation, or own name
- Flattened affect
- Circumstantial, circumlocutory, or stereotyped speech
- Speech intermittently illogical, obscure, or irrelevant
- Difficulty in understanding complex commands
- Impaired judgment
- Impaired abstract thinking
- Gross impairment in thought processes or communication
- Disturbances of motivation and mood
- Difficulty in establishing and maintaining effective work and social relationships
- Difficulty adapting to stressful circumstances, including work or a work-like setting
- Inability to establish and maintain effective relationships
- Suicidal ideation
- Obsessional rituals which interfere with routine activities
- Impaired impulse control, such as unprovoked irritability with periods of violence
- Spatial disorientation
- Persistent delusions or hallucinations
- Grossly inappropriate behavior
- Persistent danger of hurting self or others
- Neglect of personal appearance and hygiene
- Intermittent inability to perform activities of daily living, including maintenance of minimal personal hygiene
- Disorientation to time or place
C&P Exam for PTSD: Tips and Strategies
After submitting your PTSD claim to the VA, one of the critical steps in the evaluation process is the Compensation and Pension (C&P) exam for PTSD.
This exam plays a crucial role in determining your VA disability rating.
Here are some tips and strategies to help you prepare and navigate the C&P exam effectively:
Understanding the Purpose of the C&P Exam
A C&P exam for PTSD is designed to evaluate four main areas:
- Determine if you have a PTSD diagnosis that conforms to DSM-5.
- Validate the PTSD stressor event. The stressful event can be due to combat, personal trauma, or other life-threatening situations (non-combat-related stressors). The key element for a valid PTSD stressor event is whether a veteran feared for their life.
- The examiner will provide their medical opinion on whether your PTSD was caused or made worse by your active duty military service or another service-connected condition. This is only for initial PTSD claims. If you already have a rating for PTSD, the examiner will not give a medical opinion for service connection.
- Assess the severity of your PTSD symptoms in terms of frequency, severity, and duration, and their negative impact on your occupational and social impairment.
Be Uncomfortably Vulnerable
During the exam, it’s essential to be uncomfortably vulnerable and provide a complete picture of the severity of your PTSD symptoms.
Describe your experiences in detail, including how often symptoms occur, their severity, and their impact on your daily activities.
Do not downplay your symptoms, even if you feel embarrassed or uncomfortable discussing them.
This is your chance to tell all so don’t hold back!
Know the VA’s PTSD Symptoms and Their Impact
The VA evaluates PTSD based on 31 specific mental health symptoms from the DBQ form, and their impact on your work, life, and social functioning.
Familiarize yourself with common PTSD markers, such as flashbacks, nightmares, hypervigilance, avoidance behaviors, and mood disturbances.
Be ready to discuss symptoms such as anxiety, depression, anger, panic attacks, sleep issues, memory loss, OCD-like behaviors, etc.
Be prepared to discuss how these symptoms impact your occupational and social impairment.
Discuss Occupational and Social Impairment
Explain how PTSD has affected your ability to work and maintain relationships.
For example, if you’ve had to change jobs, take leave, or reduce hours due to PTSD symptoms, mention this.
Also, discuss any challenges you face in social settings, maintaining friendships, or family dynamics.
Be Prepared for a Wide Range of Questions
During a C&P exam for PTSD, the examiner will ask a bunch of questions from the DBQ for PTSD.
Here’s some common mental health C&P exam questions you may encounter:
- Do you have a PTSD diagnosis that aligns with DSM-5 criteria?
- Describe your PTSD symptoms in-detail.
- How do your PTSD symptoms impact your work, life, and social functioning?
- Describe any periods of severe symptoms and their negative impacts.
- Provide a brief overview of your military, social, marital, and family history.
- What is your background including educational and work history?
- Describe any specific traumatic events that led to the development of your PTSD.
- Describe the traumatic events and their symptoms, such as distressing memories, dreams, or flashbacks.
- Do you avoid reminders of the events?
- How long have these symptoms persisted?
- Discuss symptoms like depression, anxiety, sleep issues, memory loss, and their frequency.
- How do you behave in social settings and daily activities?
- Are there any additional symptoms not listed?
Is the VA Changing How It Rates PTSD?
Yes, significant updates to the VA mental health rating criteria are expected by the end of 2026.
Here are the key updates under the new VA mental health rating criteria:
Domain-Based Assessment
The new rating system will evaluate mental health conditions across five key domains:
- Cognition: The ability to think, understand, and remember.
- Interpersonal Interactions and Relationships: The ability to interact with others and maintain relationships.
- Task Completion: The ability to perform and complete tasks, both personal and vocational.
- Life Activities and Navigating Environments: The ability to engage in daily life activities and move through different environments.
- Self-Care: The capacity to care for oneself independently.
Minimum Rating Change
The minimum VA disability rating for mental health conditions will increase from 0% to 10%; there is no more 0% rating for mental health.
This change acknowledges that even milder symptoms can still affect a veteran’s life and deserve compensation.
Elimination of Work-Based Restrictions
The VA will remove the current restriction that prevents veterans from receiving a 100% rating for a mental health condition if they are still able to work.
This change aims to provide more accurate compensation for veterans who are severely impaired but can still manage some level of employment.
More Generous Disability Compensation
The new criteria are designed to offer more generous compensation by focusing on the functional impairment caused by mental health conditions, rather than just the number and type of symptoms present in a subjective assessment.
The changes will allow for higher ratings for mental health conditions with less stringent requirements for the 70% and 100% VA rating criteria.
MASSIVE VA Rating Changes to Mental Health Conditions (Short Video)
The biggest changes to VA ratings for mental health conditions, including PTSD, depression, anxiety, and adjustment disorder, are upon us.
Find out what’s changing and what’s staying the same in this 3-minute video by Brian Reese:
About the Author

Brian Reese
Brian Reese is a world-renowned VA disability benefits expert and the #1 bestselling author of VA Claim Secrets and You Deserve It. Motivated by his own frustration with the VA claim process, Brian founded VA Claims Insider to help disabled veterans secure their VA disability compensation faster, regardless of their past struggles with the VA. Since 2013, he has positively impacted the lives of over 10 million military, veterans, and their families.
A former active-duty Air Force officer, Brian has extensive experience leading diverse teams in challenging international environments, including a combat tour in Afghanistan in 2011 supporting Operation ENDURING FREEDOM.
Brian is a Distinguished Graduate of Management from the United States Air Force Academy and earned his MBA from Oklahoma State University’s Spears School of Business, where he was a National Honor Scholar, ranking in the top 1% of his class.
Content Reviewed By
Quality Assurance Team
The Quality Assurance (QA) team at VA Claims Insider has extensive experience researching, fact-checking, and ensuring accuracy in all produced content. The QA team consists of individuals with specialized knowledge in the VA disability claims adjudication processes, laws and regulations, and they understand the needs of our target audience. Any changes or suggestions the QA team makes are thoroughly reviewed and incorporated into the content by our writers and creators.