Looking for Expert-Level VA Claim Answers?📱Call Us Now! 737-295-2226
In this post, we will be exploring how to get a VA Disability Rating for Degenerative Disc Disease.
I’ll also reveal 3 new insider tips to increase your VA Rating for Degenerate Disc Disease, even if you’ve already filed or been denied.
So, let’s take a minute to explore the law regarding the symptoms and impairment required to warrant a VA rating for Degenerative Disc Disease.
Many veterans suffer from various back conditions due to their military service, including Degenerative Disc Disease.
A VA disability rating for Degenerative Disc Disease can be rated at 10%, 20%, 30%, 40%, 50%, or 100%.
Your final VA disability rating for Degenerative Disc Disease depends upon the frequency, severity, and duration of your symptoms, including Painful Motion, Limitation of Range of Motion (ROM), and Functional Loss or Impairment.
In addition, numerous research studies have shown a link between Degenerative Disc Disease and Radiculopathy; there is a strong bidirectional relationship where each disorder adversely influences the other one.
Furthermore, Depression is one of the most common comorbidities in veterans with chronic low back pain.
- What is Degenerative Disc Disease in Veterans?
- Common Signs and Symptoms of Degenerative Disc Disease in Veterans
- VA Disability Rating for Degenerative Disc Disease: Basic Eligibility Criteria
- What is the Degenerative Disc Disease VA Rating?
- VA Rating for Degenerative Disc Disease – 10% to 100%
- Common VA Secondary Conditions to Degenerative Disc Disease
- Frequently Asked Questions (FAQs): VA Disability for Degenerative Disc Disease
- What is the “Painful Motion” Principle?
- Full definition of Painful Motion
- What is “Limitation of Range of Motion” for VA Degenerative Disc Disease?
- Accurate Measurement of Limitation of Range of Motion
- What is “Functional Loss” in a VA disability claim for Degenerative Disc Disease ?
- Functional Loss Full Definition
- Do You Deserve a Higher VA Disability Rating?
- About the Author
What is Degenerative Disc Disease in Veterans?
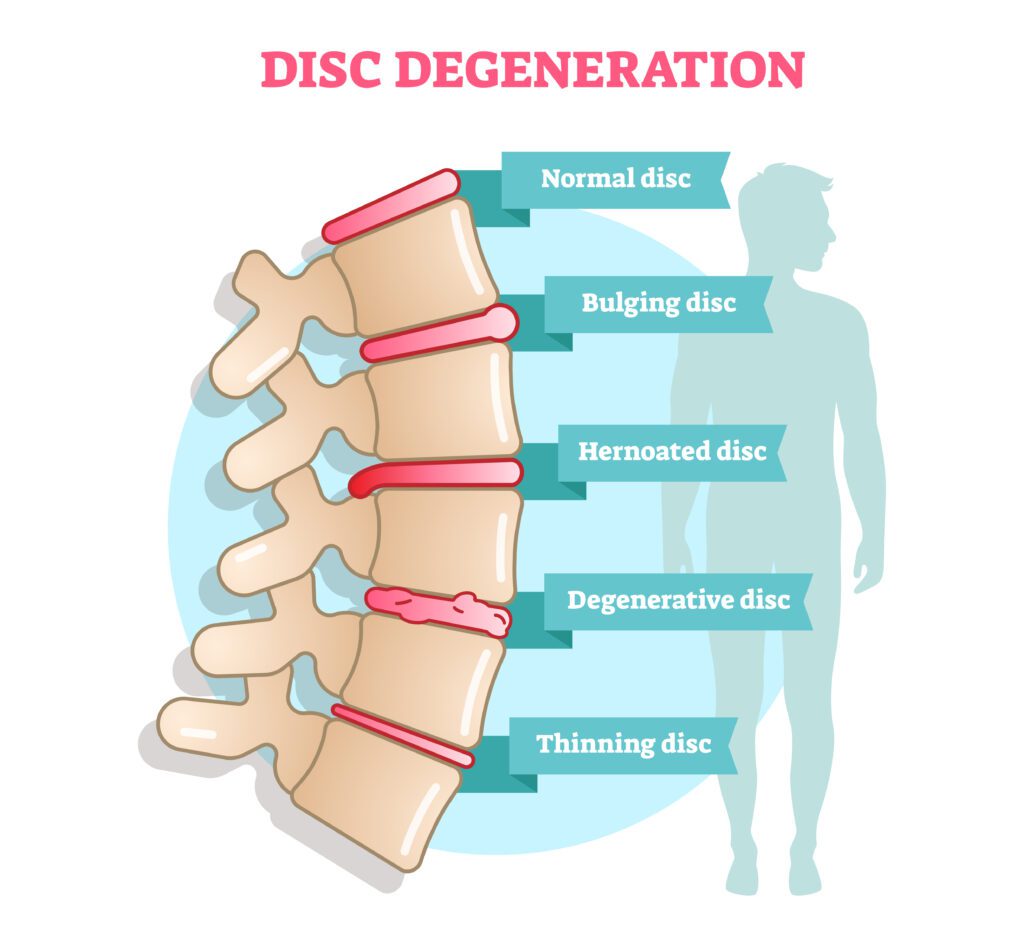
Degenerative Disc Disease is a painful spinal disorder caused by the steady degeneration of the intervertebral discs, which are the pads that cushion the bones in the vertebrae of your spine.
With age or trauma, the intervertebral discs lose their water content, leaving the discs more prone to tearing or damage. Thinner and weaker discs often lead to back pain, muscle weakness, and pinched nerves.
Degenerative Disc Disease is one of the most common causes of low back (lumbar), mid back (thoracic), and neck pain (cervical) in veterans.
In more severe cases, Degenerative Disc Disease can cause weakness, numbness, and shooting or throbbing pain in the arms or legs, which is a painful condition known as Radiculopathy.
Common Signs and Symptoms of Degenerative Disc Disease in Veterans

A few of the risk factors for Degenerative Disc Disease include your age, prior back injuries, car accidents, being overweight or obese, a sedentary lifestyle, or other forms of bodily trauma.
Generally, some of the more common symptoms of Degenerative Disc Disease include:
- Pain that worsens when sitting (while seated, the discs of the lower back have 3x more load on them than when standing).
- Pain that worsens when standing, bending, lifting, or twisting.
- Feeling better while walking or even running than while sitting or standing for long periods of time.
- Feeling better by changing positions often or lying down.
- Periods of severe pain that come and go. These can last from a few days to a few months before getting better. They can range from dull nagging pain to severe disabling (sharp or throbbing) pain.
- Pain in the low back (lumbar), mid back (thoracic), or neck (cervical), depending on where the affected disc is, possibly even radiating to the legs, arms, and hands (Radiculopathy).
- Pain, numbness, weakness, or tingling in the extremities.
VA Disability Rating for Degenerative Disc Disease: Basic Eligibility Criteria

VA Disability Rating for Degenerative Disc Disease
To be eligible for a Degenerative Disc Disease VA rating, a veteran must meet three (3) criteria by law:
- #1. Medical diagnosis of Degenerative Disc Disease in a medical record (Service Treatment Records, VA medical records, or private medical records)
- #2. Your Degenerative Disc Disease was caused or made worse by your active-duty military service OR by another service-connected disability for secondary service connection (“Nexus” for service connection)
- #3. Persistent and recurring symptoms of Degenerative Disc Disease (“Severity of Symptoms”)
If you think you have a back condition, such as Degenerative Disc Disease, but don’t have a medical diagnosis, pick up the phone and call the VA mental health facility nearest you to make an appointment right away!
If you’re trying to increase your VA disability rating for Degenerative Disc Disease, you need to prove to the VA that your symptoms are now worse and warrant a higher rating by law.
The #1 best way to increase your Degenerative Disc Disease VA disability rating is to get X-Rays so you have objective medical evidence to show the degradation of your discs over time.
(1) Limitation of Range of Motion and (2) Pain are the two most common factors that determine your final VA rating for back conditions such as Degenerative Disc Disease.
What is the Degenerative Disc Disease VA Rating?

A VA disability rating for Degenerative Disc Disease can be rated at 10%, 20%, 30%, 40%, 50%, or 100% depending upon the Frequency, Severity, and Duration of your symptoms.
Degenerative Disc Disease is a spinal disorder most often rated under CFR Title 38, Part 4, VA Schedule of Ratings, Diagnostic Code 5242, Degenerative Arthritis, Degenerative Disc Disease Other Than Intervertebral Disc Syndrome.
VA Rating for Degenerative Disc Disease – 10% to 100%
| DC 5242, Degenerative Arthritis, Degenerative Disc Disease Other Than Intervertebral Disc Syndrome | VA Rating |
| Unfavorable ankylosis of the entire spine | 100% |
| Unfavorable ankylosis of the entire thoracolumbar spine | 50% |
| Unfavorable ankylosis of the entire cervical spine; or forward flexion of the thoracolumbar spine 30 degrees or less; or favorable ankylosis of the entire thoracolumbar spine | 40% |
| Forward flexion of the cervical spine 15 degrees or less; or favorable ankylosis of the entire cervical spine | 30% |
| Forward flexion of the thoracolumbar spine greater than 30 degrees but not greater than 60 degrees; or, forward flexion of the cervical spine greater than 15 degrees but not greater than 30 degrees; or, the combined range of motion of the thoracolumbar spine not greater than 120 degrees; or, the combined range of motion of the cervical spine not greater than 170 degrees; or, muscle spasm or guarding severe enough to result in an abnormal gait or abnormal spinal contour such as scoliosis, reversed lordosis, or abnormal kyphosis | 20% |
| Forward flexion of the thoracolumbar spine greater than 60 degrees but not greater than 85 degrees; or, forward flexion of the cervical spine greater than 30 degrees but not greater than 40 degrees; or, combined range of motion of the thoracolumbar spine greater than 120 degrees but not greater than 235 degrees; or, combined range of motion of the cervical spine greater than 170 degrees but not greater than 335 degrees; or, muscle spasm, guarding, or localized tenderness not resulting in abnormal gait or abnormal spinal contour; or, vertebral body fracture with loss of 50 percent or more of the height | 10% |
| Evaluate intervertebral disc syndrome (preoperatively or postoperatively) either under the General Rating Formula for Diseases and Injuries of the Spine or under the Formula for Rating Intervertebral Disc Syndrome Based on Incapacitating Episodes, whichever method results in the higher evaluation when all disabilities are combined under §4.25. |
Common VA Secondary Conditions to Degenerative Disc Disease

- Radiculopathy
- Depression
- Anxiety
- Somatic Symptom Disorder
- Musculoskeletal Conditions (e.g., back, neck, hips, feet)
- Osteoarthritis
- Scoliosis
- Spinal Stenosis
- Spondylolisthesis
- Spondylolysis
- GERD and IBS
- Plantar Fasciitis
Frequently Asked Questions (FAQs): VA Disability for Degenerative Disc Disease
What is the “Painful Motion” Principle?
The painful motion principle means that regardless of range of motion, if pain is present, the claimant should at least be awarded the minimum level of disability for that condition.
For example, let’s say you have full range of motion for your Degenerative Disc Disease, but you have pain during movement, you should be awarded the minimum level of disability for the condition, which is 10%.
Full definition of Painful Motion
With any form of arthritis, painful motion is an important factor of disability, the facial expression, wincing, etc., on pressure or manipulation, should be carefully noted and definitely related to affected joints.
Muscle spasm will greatly assist the identification.
Sciatic neuritis is not uncommonly caused by arthritis of the spine.
The intent of the schedule is to recognize painful motion with joint or periarticular pathology as productive of disability.
It is the intention to recognize painful, unstable, or malaligned joints, due to healed injury, as entitled to at least the minimum compensable rating for the joint.
Crepitation either in the soft tissues such as the tendons or ligaments, or crepitation within the joint structures should be noted carefully as points of contact which are diseased.
Flexion elicits such manifestations.
The joints involved should be tested for pain on both active and passive motion, in weight-bearing and non-weight-bearing and, if possible, with the range of the opposite undamaged joint.
What is “Limitation of Range of Motion” for VA Degenerative Disc Disease?
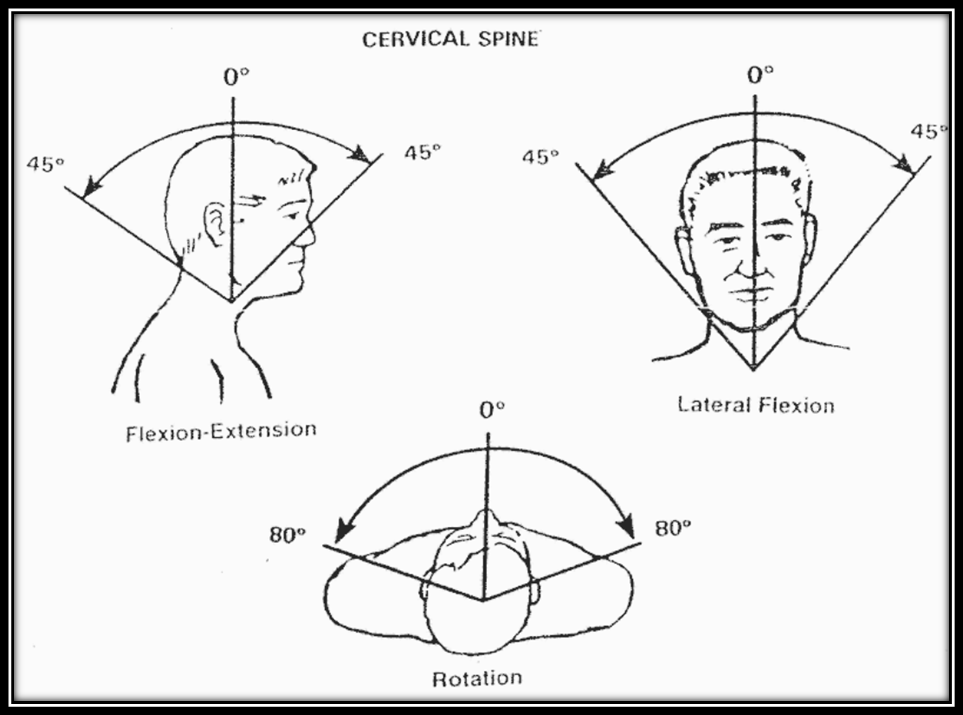
The limitation of range of motion principle is arguably the most important principle that applies to VA disability ratings for back pain and Degenerative Disc Disease.
Why?
Because the general rating formula for diseases and injuries of the spine talk about “flexion,” which is the act of flexing or bending.
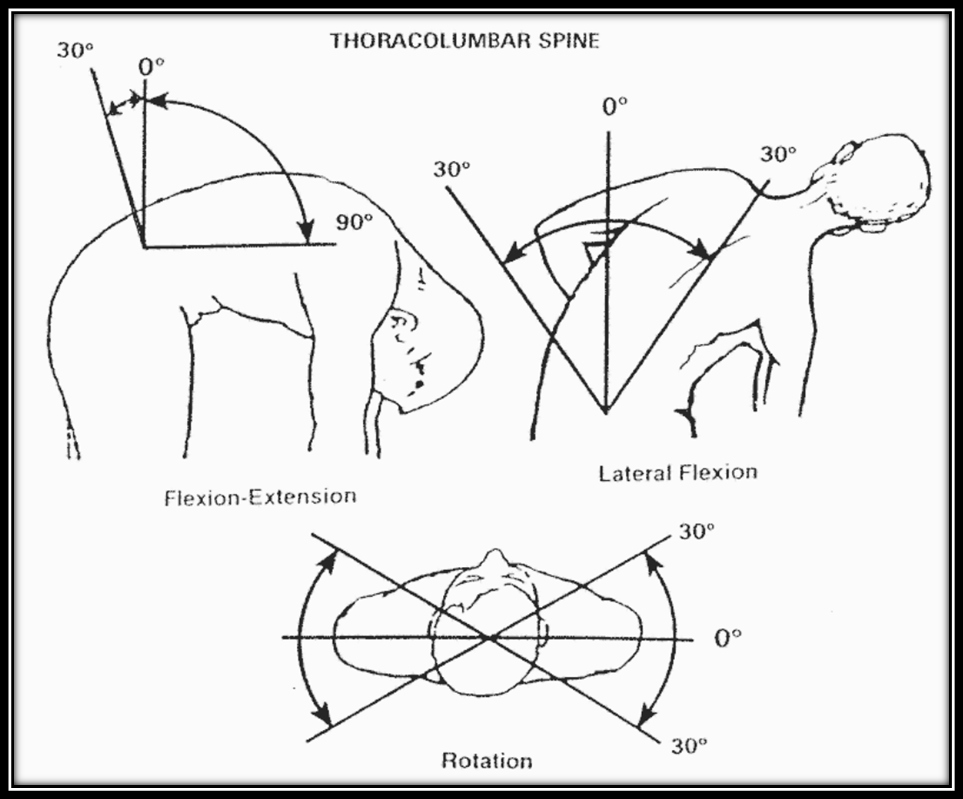
Any limitation of Range of Motion (ROM) should be measured with a Goniometer by the medical professional at your VA C&P Exam for Back Pain.
You must be open, honest, and truthful at your C&P exam for Degenerative Disc Disease, and make sure to STOP the C&P examiner as soon as you feel any discomfort or pain.
If you can’t move at all without discomfort or pain, make sure to let the examiner know that.
Accurate Measurement of Limitation of Range of Motion
Accurate measurement of the length of stumps, excursion of joints, dimensions, and location of scars with respect to landmarks, should be insisted on.
The use of a goniometer in the measurement of limitation of motion is indispensable in examinations conducted within the Department of Veterans Affairs.

Muscle atrophy must also be accurately measured and reported.
You’ll also see the term “Unfavorable Ankylosis,” which is a condition in which the entire cervical spine, the entire thoracolumbar spine, or the entire spine is fixed in flexion or extension, and the ankylosis results in one or more of the following:
- Difficulty walking because of a limited line of vision
- Restricted opening of the mouth and chewing
- Breathing limited to diaphragmatic respiration
- Gastrointestinal symptoms due to pressure of the coastal margin on the abdomen
- Dyspnea or dysphagia
- Alantoaxial or cervical subluxation or dislocation
- Neurologic symptoms due to nerve root stretching
What is “Functional Loss” in a VA disability claim for Degenerative Disc Disease ?
VA disability ratings for Degenerative Disc Disease also depend upon “Functional Loss,” which means impairment of spine function as determined by range of motion as reported in the physical examination and additional loss of range of motion after repetitive use caused by the following factors:
- #1. Pain
- #2. Fatigue
- #3. Weakness
- #4. Lack of endurance
- #5. Incoordination
Functional Loss Full Definition
VA disability of the musculoskeletal system is primarily the inability, due to damage or infection in parts of the system, to perform the normal working movements of the body with normal excursion, strength, speed, coordination and endurance.
It is essential that the examination on which ratings are based adequately portray the anatomical damage, and the functional loss, with respect to all these elements.
The functional loss may be due to absence of part, or all, of the necessary bones, joints and muscles, or associated structures, or to deformity, adhesions, defective innervation, or other pathology, or it may be due to pain, supported by adequate pathology and evidenced by the visible behavior of the claimant undertaking the motion.
Weakness is as important as limitation of motion, and a part which becomes painful on use must be regarded as seriously disabled.
A little used part of the musculoskeletal system may be expected to show evidence of disuse, either through atrophy, the condition of the skin, absence of normal callosity or the like.
Do You Deserve a Higher VA Disability Rating?
At VA Claims Insider, we help fellow Veterans celebrate LIFE CHANGE by getting them the VA disability rating and compensation YOU DESERVE by law.
And, you’ll get to work with a Veteran Coach (VC) who will lead you to VA claim success.
- We’re a company OF Veterans, BY Veterans, FOR Veterans! FOR Veterans, BY Veterans. We’re the largest community of Veterans Helping Veterans Worldwide™
- 25,000+ disabled veterans served in our Elite Membership program since 2016 with and average VA disability rating increase of >30%
- 4.8/5.0 Google Reviews rating across 2,000+ total reviews
Click HERE to Join the #1 Rated VA Claims Insider Elite Program and Start Today for FREE.
About the Author

Brian Reese
Brian Reese is a world-renowned VA disability benefits expert and the #1 bestselling author of VA Claim Secrets and You Deserve It. Motivated by his own frustration with the VA claim process, Brian founded VA Claims Insider to help disabled veterans secure their VA disability compensation faster, regardless of their past struggles with the VA. Since 2013, he has positively impacted the lives of over 10 million military, veterans, and their families.
A former active-duty Air Force officer, Brian has extensive experience leading diverse teams in challenging international environments, including a combat tour in Afghanistan in 2011 supporting Operation ENDURING FREEDOM.
Brian is a Distinguished Graduate of Management from the United States Air Force Academy and earned his MBA from Oklahoma State University’s Spears School of Business, where he was a National Honor Scholar, ranking in the top 1% of his class.



