Looking for Expert-Level VA Claim Answers?📱Call Us Now! 737-295-2226
If you are a veteran with narcolepsy, you are not alone. Falling asleep instantly, extreme daytime sleepiness, and uneven or interrupted sleep throughout the night are common symptoms for the nearly 200,000 people diagnosed with narcolepsy in the United States.
In this post, we’ll break down how the VA determines narcolepsy VA disability ratings, what the different possible narcolepsy ratings are, how to prove service connection, and more.
Table of Contents

Summary of Key Points
- Narcolepsy VA ratings are 0%, 10%, 20%, 40%, 60%, 80%, and 100%, depending on the severity and frequency of symptoms.
- The VA uses the same rating scale as is used for seizures when rating narcolepsy.
- Service connection is mandatory to receive a VA rating for narcolepsy.
What Is Narcolepsy?
Narcolepsy is a chronic (i.e., long-term) neurological disorder that affects the brain’s ability to control sleep-wake cycles. The condition involves extreme daytime drowsiness (hypersomnolence) and falling asleep suddenly.
People with narcolepsy often have trouble staying asleep at night. They often fall asleep regardless of how much sleep they get at night— anytime, anywhere (even during normal daytime activities). These symptoms can significantly interfere with daily life.
Narcolepsy Symptoms
Symptoms of narcolepsy that negatively impact sleep quality include:
- Sleep paralysis – a temporary inability to move or speak while falling asleep or waking up
- Quickly falling into REM sleep (i.e., a deep sleep stage in which most dreaming occurs), which may even happen during the day
- Sleep fragmentation – brief, repeated interruptions that prevent deep sleep stages
- Hypnagogic hallucinations – seeing or hearing things that aren’t real or feeling sensations that are not there; can include vivid or frightening visual, auditory, or tactile (i.e., sense of touch) sensations that occur when you’re falling asleep.
- Hypnopompic hallucinations – visual, auditory, or tactile sensations that aren’t real that occur when you awaken; these hallucinations often involve a continuation of dreams after you wake up.
- Cataplexy (i.e., a sudden loss of muscle tone)
What Is Cataplexy?
Cataplexy is considered a critical factor in rating narcolepsy. Common symptoms of cataplexy include:
- A sudden loss of muscle tone (which may include slurred speech)
- Falling due to a sudden loss of leg muscle strength
- Sleep paralysis
- Symptoms triggered by intense emotions such as fear, anger, or laughing
- Symptoms that last up to a few minutes and may involve several episodes a day
Over the first few years of narcolepsy, the condition often worsens, stabilizes, and then the condition may worsen again.
Two Types of Narcolepsy
There are two distinct types of narcolepsy, including:
- Type I Narcolepsy – involves cataplexy; this is the most common type of narcolepsy among those with cataplexy, and it involves low hypocretin (a brain hormone) levels. Intense emotions, such as laughter, excitement, laughter, anger, surprise, or frustration, can trigger this type of narcolepsy.
- Type 2 Narcolepsy – involves normal hypocretin levels and excessive daytime sleepiness without cataplexy
Note: The VA Narcolepsy Disability Benefits Questionnaire does not ask whether you are diagnosed with type one or type two narcolepsy. Instead, the Narcolepsy VA disability rating is based on the impact of the condition on each individual veteran’s daily life, specifically, the frequency and severity of the symptoms the veteran experiences.
Causes of Narcolepsy
Common causes of narcolepsy include:
- Low hypocretin levels
- Genetic factors
- Autoimmune reaction
- Infections (e.g., H1N1 virus and vaccine)
- Environmental triggers (e.g., stress, changes in sleep habits such as those experienced in the military))
VA Ratings for Narcolepsy
Narcolepsy VA ratings are 10%, 20%, 40%, 60%, 80%, or 100%, depending on the severity and frequency of your symptoms.
The VA rates narcolepsy according to 38 CFR § 4.124a, Schedule of Ratings. According to diagnostic code 8108, narcolepsy should be rated under the same guidelines as epilepsy, petit mal DC 8911. The specific VA ratings criteria are below. As you read them, keep in mind the relevant notes as well.
Note (1): A major seizure is characterized by a generalized tonic-clonic convulsion with unconsciousness.
Note (2): A minor seizure consists of a brief interruption in consciousness or conscious control associated with staring or rhythmic blinking of the eyes or nodding of the head (“pure” petit mal), or sudden jerking movements of the arms, trunk, or head (myoclonic type) or sudden loss of postural control (akinetic type).
The VA rates narcolepsy according to the severity of seizure-like symptoms. These uncontrollable episodes are like seizures in how they impact a person’s functioning; they can lead to changes in consciousness as well as present safety issues. Therefore, the VA uses the same rating criteria for narcolepsy VA disability as it does for epilepsy.
Keep in mind that medically, epilepsy and narcolepsy are distinct conditions.
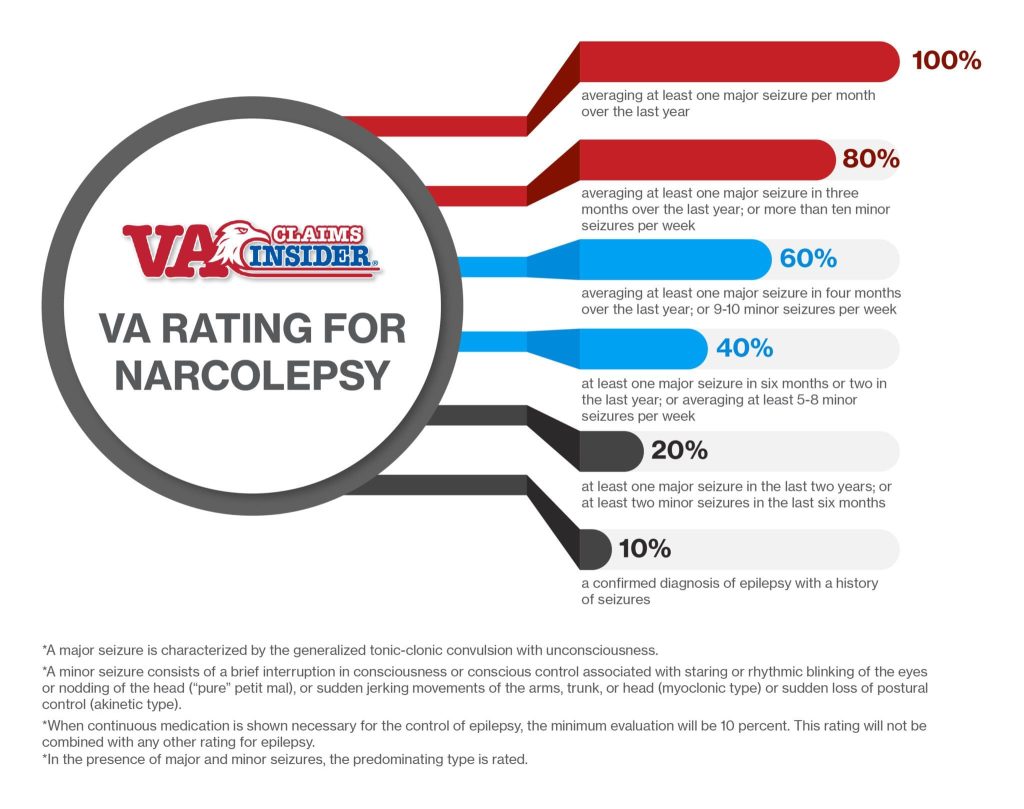
Narcolepsy VA Disability Rating Table
The table below shows VA ratings for seizure-like symptoms often experienced with narcolepsy.
| Seizure Episodes | VA RATING |
| A confirmed diagnosis of narcolepsy with a history of seizures | 10% |
| At least 2 minor seizures in the last 6 months or at least one major seizure in the last 2 years | 20% |
| At least 1 major seizure in the last 6 months or 2 in the last year or averaging at least 5 to 8 minor seizures weekly | 40% |
| Averaging at least 1 major seizure in 4 months over the last year; or 9–10 minor seizures per week | 60% |
| Averaging at least 1 major seizure in 3 months over the last year or more than 10 minor seizures weekly | 80% |
| Averaging at least 1 major seizure per month over the last year | 100% |
Note: If you require continuous medication to control your symptoms, such as antidepressants to treat symptoms of cataplexy, hallucinations, and sleep paralysis, the minimum rating you would receive for narcolepsy is 10%.
VA Disability, Narcolepsy, and Seizures, What’s the Link?
When you look at the VA rating scale for narcolepsy, you may be surprised to see that the ratings are focused on how many seizures you have in a given time span. At first glance, you may think you’ve clicked on the wrong scale, but this is how the VA rates narcolepsy; why?
The VA considers severe narcolepsy episodes involving cataplexy comparable to ratings under the 38 CFR § 4.124a schedule of ratings for minor seizures because, like seizures, narcolepsy episodes can cause brief consciousness disruptions (similar to “petit mal” or “absence seizures”).
Note: A petit mal/absence seizure is a type of seizure that involves brief periods of staring or zoning out instead of twitching or convulsing
As part of the VA’s disability rating process, the reviewer will assess the frequency and severity of narcoleptic episodes involving cataplexy.
Narcolepsy VA Disability Compensation: What’s Required?
Requirements for a VA narcolepsy rating include the following:
- Having a current diagnosis of narcolepsy performed by a licensed healthcare provider
- Proving military service connection (e.g., an injury, illness, or event related to your condition that occurred during your military service)
- Obtaining a sleep study showing the quality of your sleep that indicates signs of narcolepsy
- Showing differentiation between narcolepsy and other sleep disorders or conditions
Proving Service Connection
If you can prove your disorder is service-connected (i.e., caused or worsened by your military service), you may qualify for disability compensation.
When you file a narcolepsy VA claim, a reviewer will look for evidence showing that your condition is connected to your military service, such as a medical connection between your diagnosis and a related injury, illness, or event during your military service.
Your military records, including disciplinary action notations, could help support service connection for your sleep disorder. Service-connected “events” that can help support your disability claim may include sleep-related disciplinary violations, like falling asleep during formation, field duty during daytime hours, or in the mess hall (i.e., DEFAC).
Direct Service Connection
- Narcolepsy is typically a primary condition. To prove direct service connection, you will need to show that your narcolepsy began during or after active duty and that it is the result of an injury or event that occurred during service.
Secondary Service Connection
Narcolepsy is not typically secondary to another service-related condition. To prove secondary service connection, you will need to show that you have a service-connected condition and that this condition has caused or aggravated your narcolepsy.
Secondary Conditions to Narcolepsy
Other sleep disorders are commonly linked with narcolepsy, such as:
- Sleep apnea without cataplexy – the most common sleep disorder secondary to narcolepsy)
- REM sleep behavior disorder (RBD) – physically acting out vivid dreams during REM sleep
- Insomnia – a sleep disorder and a common narcolepsy symptom that is often worsened by narcolepsy
Some veterans experience mental health symptoms like anxiety and depression as a result of chronic narcolepsy. If a healthcare provider finds a link between your mental health symptoms and your service-connected narcolepsy diagnosis, you may qualify for a secondary condition rating. The VA uses a Combined Rating Table to assess your disability compensation when you have a secondary service-connected condition.
Obesity and Narcolepsy
In addition to mental health disorders, recent studies, including a 2022 study, show a link between sudden weight gain and narcolepsy. Experts surmise that this sudden weight gain is due to a decrease in metabolism from inactivity while sleeping. Obesity is commonly linked with other disorders, such as diabetes and high blood pressure.
If you receive a service-connected narcolepsy VA rating resulting in significant weight gain, an obesity diagnosis along with related disorders (e.g., hypertension or diabetes) could result in a causal chain of various secondary conditions that qualify for VA disability ratings.
Narcolepsy and TDIU
If you are unable to maintain “substantially gainful employment” because of your service-connected narcolepsy, you may qualify for Total Disability Based on Individual Unemployability (TDIU). TDIU involves a total disability rating, regardless of whether your VA rating for narcolepsy is less than 100%
(FAQs) Frequently Asked Questions
How does the VA rate narcolepsy?
Narcolepsy is rated by the VA using the General Rating Formula for epileptic seizures. VA narcolepsy ratings are 10%, 20%, 40%, 60%, 80%, or 100%, depending on the severity and frequency of your symptoms.
Is it difficult to get narcolepsy VA disability?
Getting a VA disability rating for narcolepsy can be challenging. You must show a service connection by proving that an accident, illness, or event linked with narcolepsy occurred during your military service. It’s sometimes difficult to differentiate between narcolepsy symptoms and other sleep disorders or conditions; therefore, a diagnostic test, such as a sleep study, may be needed.
What symptoms are considered when the VA rates narcolepsy?
Symptoms of narcolepsy that impact a person’s functioning and ability to work are often similar to petit mal seizures. Therefore, the VA rating scale, used to evaluate narcolepsy symptoms, is the same as the petit mal seizure rating scale.
Does the VA consider narcolepsy a presumptive condition?
No, narcolepsy is not considered a presumptive condition; you must show that your narcolepsy was caused or worsened by your military service to get rated for VA disability compensation.
Are there any additional narcolepsy complications veterans experience?
Military members who serve in the Army, Navy, Marines, Air Force, and Coast Guard can experience symptoms of narcolepsy due to deployment-related stress. Veterans may experience other complications related to and conditions caused by the disorder, including moodiness, irritability, anxiety, memory difficulties, inability to concentrate, depression, withdrawal from social activities, paranoia, or changes in REM sleep.
Want Expert-Level VA Disability Claim Help? WE GOT YOUR SIX!
- VA Claims Insider is the #1 most trusted name in VA disability claims.
- Work directly with a VA claims coach who can guide you to VA claim victory.
- 25,000+ disabled veterans served in our membership programs since 2016.
- 30% average rating increase for veterans who complete our #1 rated Elite program.
- 4.7/5.0 average rating out of 5,500+ total reviews; over 4,500 5-star reviews.

Sherry Christiansen
Sherry Christiansen is a professional Medical Writer with a clinical mental health background. Over the last decade, she has written health and wellness articles for organizations like Medical News Today, Verywell Health, and Healthline. In 2013, she also helped launch an educational website for the first Alzheimer’s prevention clinic in the country at Weill Cornell Medical Center – NewYork-Presbyterian. As a spouse of a career military service member, Sherry is deeply passionate about supporting veterans. It is an honor for her to assist veterans in receiving the benefits they deserve after becoming ill or injured while serving our country.


