Looking for Expert-Level VA Claim Answers?📱Call Us Now! 737-295-2226
Living with gastroparesis can be uncomfortable, painful, and even embarrassing.
But if you can link your gastroparesis to your military service, either directly, secondary to another service-related condition, or by aggravation, you may qualify for a gastroparesis VA rating up to 80%.
In this post, we’ll break down the VA rating for gastroparesis, what benefits you may be eligible for, and how to file your claim.
Summary of Key Points
- A gastroparesis VA rating can range from 0% to 80%, depending on the severity of your symptoms and their impact on your daily life and work.
- You must show your gastroparesis is connected to your military service, either directly, secondarily (e.g., due to service-connected diabetes), or through aggravation.
- You can file your VA claim online at VA.gov, by mail, fax, or in person at a VA regional office. If you need support, consider a VA Claim Discovery Call.
Table of Contents
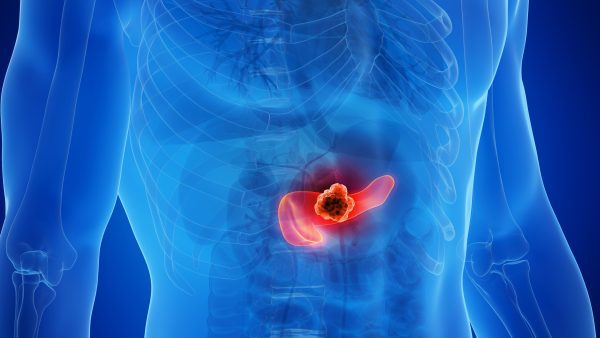
Gastroparesis in Veterans
Gastroparesis, also known as delayed gastric emptying, is a condition where the stomach muscles don’t work properly, slowing or stopping the movement of food from the stomach to the small intestine. According to the Mayo Clinic, this can lead to symptoms like:
- Nausea and vomiting
- Abdominal pain and bloating
- Feeling full after eating small amounts
- Acid reflux
- Changes in blood sugar
- Loss of appetite, weight loss, and malnutrition
The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) notes that diabetes is the most common cause of gastroparesis, which is particularly relevant for veterans since diabetes is prevalent among us due to factors like Agent Orange exposure.
Veterans may be at higher risk for gastroparesis due to service-related conditions. For instance, medications for post-traumatic stress disorder (PTSD) or pain (like opioids) can contribute, as can surgeries or viral infections experienced during deployment.
The Veterans Health Library explains that causes of gastroparesis include diabetes, digestive surgeries, certain medicines, hypothyroidism, nervous system disorders, autoimmune diseases, viral stomach infection, or unknown factors.
Treatments include dietary changes, blood sugar control for diabetics, medications to improve stomach motility, or, in severe cases, feeding tubes or surgery.
How the VA Rates Gastroparesis
Gastroparesis isn’t listed specifically in the VA’s Schedule for Rating Disabilities, so the VA rates it by analogy, often under diagnostic code (DC) 7399-7346 for hiatal hernia using the criteria for stricture of the esophagus (DC 7203).
This means your rating is based on symptoms like pain, vomiting, weight loss, and overall health impairment.
Here’s the breakdown from the VA’s rating schedule under DC 7346 (Hiatal Hernia):
| VA Rating | Stricture of the Esophagus Rating Criteria |
| 80% | Documented history of recurrent or refractory esophageal stricture(s) causing dysphagia (difficulty swallowing) with at least one of the symptoms present: (1) aspiration, (2) undernutrition, and/or (3) substantial weight loss as defined by § 4.112(a) and treatment with either surgical correction or percutaneous esophago-gastrointestinal tube (PEG tube). |
| 50% | Documented history of recurrent or refractory esophageal stricture(s) causing dysphagia which requires at least one of the following: (1) dilatation three or more times per year, (2) dilatation using steroids at least one time per year, or (3) esophageal stent placement. |
| 30% | Documented history of recurrent esophageal stricture(s) causing dysphagia that requires dilatation no more than two times per year. |
| 10% | Documented history of esophageal stricture(s) that requires daily medications to control dysphagia otherwise asymptomatic. |
| 0% | Documented history without daily symptoms or requirement for daily medications. |
For example, in one VA Board of Veterans’ Appeals decision, a veteran received a 60% rating for idiopathic gastroparesis with severe symptoms (BVA Citation 1602300). Your rating depends on how your symptoms affect occupational and social functioning.
Eligibility & Proving Service Connection
To qualify for a gastroparesis VA rating, you need to prove service connection. Gastroparesis can be service-connected directly (e.g., from military surgeries) or secondarily (e.g., to service-connected diabetes or medication side effects).
Direct Service Connection
A direct service connection requires:
- A current diagnosis of gastroparesis (from medical records or VA exam), and
- An in-service event, injury, illness, or aggravation (e.g., exposure leading to diabetes), and
- A medical nexus linking the two (often a nexus letter from a doctor).
Secondary Service Connection
Gastroparesis can be service-connected on a secondary basis if it is caused by or aggravated by an already service-connected condition.
You’ll need to obtain a nexus letter from a qualified medical professional that clearly states the gastroparesis is “at least as likely as not” caused or aggravated by the already service-connected condition.
Gastroparesis can be a secondary condition to:
- Diabetes
- Certain cancers
- Scleroderma
- Migraines, Parkinson’s disease, or multiple sclerosis
- Hypothyroidism
Pro Tip: Including Medical Evidence
Strong evidence is crucial: Include doctor reports, test results (like gastric emptying scans), service records, and lay statements describing the impact of your symptoms. A nexus letter tying it to service can also make a big difference.
C&P Exam for Gastroparesis
The VA may schedule a compensation and pension (C&P) exam. Expect questions on symptoms (nausea, vomiting, bloating), duration, treatments, and how your gastroparesis affects work/life.
It’s important to be honest. These exams assess severity under the rating criteria.
Conclusion
Gastroparesis is a VA-rated disability that impacts how your stomach muscles work to move food through your body. It can impact the quality of your daily life and cause serious health problems if left unaddressed.
The VA rates gastroparesis up to 80%, providing a significant benefit to those veterans who qualify. With a current diagnosis and the right medical evidence, you can be compensated from the VA if your gastroparesis is connected to your military service, either directly or as a secondary condition.
Do You Deserve a Higher VA Rating? WE GOT YOUR SIX!
Most veterans are underrated for their disabilities and, therefore, not getting their due compensation. At VA Claims Insider, we enable you to understand and take control of the claims process so you can get the rating and compensation you’re owed by law. Our process takes the guesswork out of filing a VA disability claim and supports you every step of the way in building a fully developed claim (FDC).
If you’ve filed your VA disability claim and have been denied or have received a low rating — or you’re unsure how to get started — reach out to us! Take advantage of a VA Claim Discovery Call. Learn what you’ve been missing so you can FINALLY get the disability rating and compensation YOU DESERVE!
FAQs | Frequently Asked Questions
Is gastroparesis a VA disability?
Yes, gastroparesis can be a VA-rated disability if you can prove that the condition is connected to your service, either directly or secondary to an already service-connected condition.
What is the VA rating for gastroparesis?
Gastroparesis is often VA-rated analogously with other digestive system disorders, such as hiatal hernia (DC 7346), which uses the stricture of the esophagus (DC 7203) rating criteria. The rating ranges from 0% to 80%, based on symptom severity.
Can gastroparesis be secondary to service-connected diabetes?
Yes. Diabetes is a leading cause of gastroparesis, so if your diabetes is service-connected, gastroparesis could be considered a secondary condition. The proper medical documentation, as well as a nexus letter from a qualified health professional, goes a long way to proving service connection.
What if my gastroparesis is rated 0%?
Even if you receive a 0% VA rating for gastroparesis, you have established service connection, which could allow future increases if symptoms worsen.
Content Reviewed By
Quality Assurance Team
The Quality Assurance (QA) team at VA Claims Insider has extensive experience researching, fact-checking, and ensuring accuracy in all produced content. The QA team consists of individuals with specialized knowledge in the VA disability claims adjudication processes, laws and regulations, and they understand the needs of our target audience. Any changes or suggestions the QA team makes are thoroughly reviewed and incorporated into the content by our writers and creators.
About the Author

Katie McCarthy
Katie McCarthy is a writer and editor with experience in daily news and digital and print magazine publishing. She honed her editorial (and firearms) skills at Guns & Ammo before helping launch Black Rifle Coffee Company’s Coffee or Die Magazine as the managing editor. She holds degrees in English (BA) and public administration (MPA). Katie is a military spouse and word nerd who enjoys reading, hiking, camping, gardening, and spending time with her family.